Secondary Hypogonadism Diagnostic Tool
| Hormone | Secondary (Central) Pattern | Primary (Testicular) Pattern |
|---|---|---|
| Total Testosterone | Low | Low |
| Free Testosterone | Low | Low |
| LH | Low or Inappropriately Normal | High |
| FSH | Low or Inappropriately Normal | High |
| Prolactin | Normal or Elevated (if prolactinoma) | Normal |
Enter hormone values and click Analyze to determine the likely cause of low testosterone.
Quick Summary
- Low testosterone with normal testicular size points to secondary hypogonadism.
- Start with serum total and free testosterone, then check LH, FSH, and prolactin.
- Typical lab pattern: low testosterone + low or inappropriately normal LH/FSH.
- If labs suggest a pituitary issue, order a pituitary MRI.
- Use the step‑by‑step algorithm to avoid misdiagnosis and unnecessary referrals.
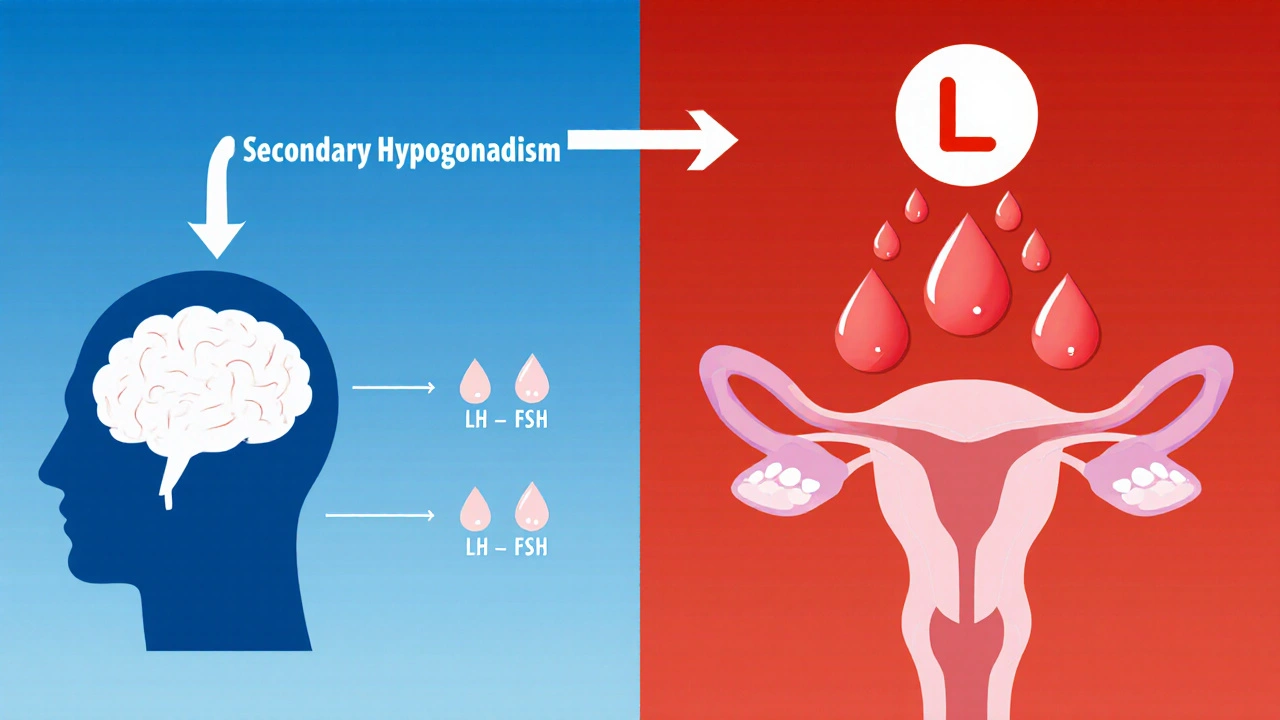
When a man shows low testosterone but the pituitary gland is the problem, that's secondary hypogonadism is a condition where the testes produce insufficient testosterone because of inadequate signaling from the brain’s hypothalamic‑pituitary axis. It’s different from primary hypogonadism, where the testes themselves are damaged. Spotting the right condition early saves time, prevents costly tests, and gets patients on the right therapy faster.
What Triggers the Need for an Evaluation?
Typical clues include:
- Persistent fatigue, low libido, or erectile dysfunction despite a normal health check.
- Weight gain, reduced muscle mass, or increased body fat.
- Blood tests that show total testosterone below 300 ng/dL (8.7 nmol/L) on at least two morning samples.
- No clear cause like chronic steroids, opioids, or severe illness.
First‑Line Hormone Tests
The backbone of the work‑up is a panel of blood tests. Below are the key players:
- Testosterone is the main male sex hormone that drives libido, muscle growth, and bone health. Measure total testosterone in the early morning (7‑10am). If total is borderline, calculate free testosterone or use equilibrium dialysis.
- Luteinizing Hormone (LH) is the pituitary hormone that tells the testes to crank out testosterone. Low or normal LH with low testosterone suggests a central problem.
- Follicle‑stimulating Hormone (FSH) is another pituitary hormone that mainly supports sperm production. In secondary hypogonadism, FSH follows the same pattern as LH.
- Prolactin is a hormone that, when elevated, can suppress GnRH and consequently LH/FSH. Elevated prolactin flags a possible prolactinoma.
Most labs also include sex hormone‑binding globulin (SHBG) because it influences free testosterone calculations.
Interpreting the Lab Results
| Hormone | Secondary (Central) Pattern | Primary (Testicular) Pattern |
|---|---|---|
| Total Testosterone | Low | Low |
| Free Testosterone | Low | Low |
| LH | Low or Inappropriately Normal | High |
| FSH | Low or Inappropriately Normal | High |
| Prolactin | Normal or Elevated (if prolactinoma) | Normal |
When LH and FSH are low while testosterone is low, the diagnosis leans toward secondary hypogonadism. An isolated low testosterone with high LH/FSH points to a primary testicular issue.
When to Move Beyond Blood Work: Imaging
If the hormone panel suggests a central problem, the next step is imaging the pituitary region. The gold standard is a contrast‑enhanced MRI.
- MRI is a magnetic resonance imaging technique that provides detailed pictures of soft tissue, including the pituitary gland. Look for micro‑adenomas (<10mm) or larger sellar masses.
- If MRI is normal but symptoms persist, consider a dynamic pituitary function test (GnRH stimulation) to unmask subtle deficiencies.
Finding a pituitary tumor changes management dramatically-often surgery or medication (e.g., dopamine agonists for prolactinomas) is required before hormone replacement.
Putting It All Together: A Step‑by‑Step Diagnostic Algorithm
- Take a thorough history focusing on sexual symptoms, energy levels, and medication use.
- Perform a physical exam-note testicular volume, body hair distribution, and any visual field deficits.
- Order morning total testosterone, free testosterone, LH, FSH, prolactin, and SHSH (optional).
- Interpret labs using the table above.
- If LH/FSH are low → suspect secondary.
- If LH/FSH are high → primary; consider genetic or autoimmune causes.
- For secondary pattern, repeat testosterone measurement in 2-4 weeks to confirm chronicity.
- Order pituitary MRI if labs remain consistent with central dysfunction.
- Refer to endocrinology when:
- MRI shows a lesion.
- Prolactin >30ng/mL.
- Patient has visual disturbances or severe headaches.
- Begin testosterone replacement only after confirming the diagnosis and ruling out contraindications (e.g., untreated prostate cancer).
Following this flow cuts down on unnecessary scans and speeds up treatment initiation.
Common Pitfalls & Red Flags
- Relying on a single testosterone draw-morning levels fluctuate, and stress can suppress results.
- Ignoring an elevated prolactin; a treatable prolactinoma can masquerade as secondary hypogonadism.
- Overlooking medications like glucocorticoids, opioids, or GnRH analogs that can suppress the axis.
- Skipping the physical exam-small testicular size suggests primary cause.
Spotting these early prevents misclassification and inappropriate hormone therapy.
Quick Checklist for Clinicians
- Ask about libido, energy, and mood.
- Measure total & free testosterone in the early morning.
- Include LH, FSH, and prolactin in the initial panel.
- Confirm low testosterone with a second morning draw.
- Interpret LH/FSH pattern to differentiate primary vs. secondary.
- Order pituitary MRI if central pattern is present.
- Refer to endocrinology for pituitary lesions, high prolactin, or unclear cases.
Frequently Asked Questions
Can lifestyle changes normalize testosterone without medication?
Improving sleep, losing excess weight, and reducing alcohol can boost testosterone modestly. However, if labs confirm secondary hypogonadism, the underlying pituitary issue won’t resolve on its own, and targeted therapy is usually needed.
Why is a pituitary MRI sometimes ordered even if prolactin is normal?
A normal prolactin level rules out prolactin‑secreting tumors, but other non‑functioning adenomas or structural lesions can still impair LH/FSH release. MRI visualizes these silent masses.
Is it safe to start testosterone therapy before a full work‑up?
Starting therapy without confirming the cause can mask an underlying tumor and delay essential treatment. Guidelines advise completing the hormone panel and MRI first, unless the patient is in acute crisis.
What testosterone level is considered low?
Most societies use 300ng/dL (8.7nmol/L) as the lower limit for total testosterone, measured in the morning on at least two occasions.
Can secondary hypogonadism be reversible?
If the cause is a treatable tumor, medication, or reversible medication effect, testosterone production often normalizes after the underlying issue is addressed. Chronic compression or irreversible pituitary damage may require lifelong hormone replacement.
By following a systematic approach-history, targeted labs, and appropriate imaging-you can confidently distinguish secondary hypogonadism from primary causes and get patients on the right treatment path.

12 Comments
Sophie Rabey
Integrating LH/FSH ratios into the diagnostic algorithm gives clinicians a robust endocrine fingerprint, even if the lab panel feels like a cocktail of acronyms-totally reassuring, right? 😏
Bruce Heintz
Great rundown! 👍 The step‑by‑step flow makes it easy to spot a central deficiency before ordering pricey MRIs.
richard king
When the hypothalamus whispers “silence” and the pituitary merely nods, the testes are left to wither in a hormonal desert. One can almost hear the echo of subdued GnRH reverberating through the cavernous folds of the brain, a lament for the lost vigor of masculinity. The lab panel, like a cryptic manuscript, lays bare the low testosterone accompanied by a meek LH, a feeble FSH-signs that the central command center has faltered. In this dim twilight, prolactin may rise like an unwelcome tide, threatening to drown the delicate feedback loops. Yet, the clinician, armed with this diagnostic compass, can navigate through the fog of nonspecific symptoms-fatigue, diminished libido, and the creeping veil of sarcopenia. By ordering a contrast‑enhanced MRI at the precise juncture, the hidden micro‑adenoma, once a silent specter, can be illuminated. If the lesion proves benign, a targeted medical therapy can coax the axis back to life, restoring the rhythmic chorus of hormones. Conversely, should the imaging reveal a more ominous mass, surgical or radiotherapeutic interventions become the only path forward. The elegance of this approach lies in its economy: avoid unnecessary tests, spare patients months of uncertainty, and allocate resources where they truly matter. Moreover, the algorithm respects the principle of “first, do no harm,” ensuring testosterone replacement is not prematurely administered, thereby masking the underlying pathology. In practice, the clinician’s empathy intertwines with evidence‑based medicine, forging a partnership with the patient that transcends mere numbers. Each morning draw, each repeat test, each nuanced interpretation becomes a stanza in the larger poem of recovery. Thus, secondary hypogonadism, once an enigmatic foe, can be demystified, managed, and perhaps even reversed, provided the underlying cause yields to treatment. The journey from suspicion to diagnosis, though fraught with potential pitfalls, is navigable with this systematic framework. Let us celebrate the power of precise endocrine diagnostics, for they restore not just hormones, but the very essence of vitality.
Dalton Hackett
The comprehensive hormone panel, when ordered in the early morning, captures the circadian peak of testosterone, thereby increasing diagnositc accuracy; however, it is essential to confirm the low value with a second draw to rule out transient fluctuations caused by acute stressors or laboratory variance. Moreover, LH and FSH should be interpreted in conjunction with SHBG levels, as alterations in binding globulin can mask true free testosterone concentrations, potentially leading to misclassification of the hypogonadal state. In cases where prolactin is modestly elevated, clinicians must consider both macroprolactin interference and true hyperprolactinemia before proceeding with dopaminergic therapy, since unnecessary medication can introduce iatrogenic complications. Imaging, specifically a contrast‑enhanced pituitary MRI, remains the gold standard for visualizing microadenomas; still, the decision to image should be guided by the hormonal pattern rather than a blanket approach, thereby avoiding undue healthcare expenditures. It is also prudent to review the patient’s medication list for agents such as opioids, glucocorticoids, or GnRH analogs, which can suppress the axis and mimic secondary hypogonadism-a factor often overlooked in routine assessments. Physical examination, with particular attention to testicular volume, provides a valuable bedside clue; a reduced size points toward a primary etiology, whereas normal dimensions support a central cause. Finally, interdisciplinary collaboration with endocrinology ensures that complex cases, especially those involving pituitary lesions or refractory hormonal derangements, receive expert management, optimizing outcomes for the patient.
William Lawrence
Oh sure, because ordering MRIs for every low testosterone is totally cost‑effective.
Grace Shaw
In adherence to the established clinical guidelines, it is incumbent upon the practitioner to first obtain at least two corroborating morning serum testosterone measurements prior to initiating any therapeutic regimen; failure to do so may result in iatrogenic complications and obscure the underlying etiology of the hypogonadal presentation. Subsequent evaluation of luteinizing hormone and follicle‑stimulating hormone concentrations should be performed concomitantly, as these indices provide indispensable insight into the functional status of the hypothalamic‑pituitary‑gonadal axis. Should the hormonal profile be indicative of a secondary pattern, namely low or inappropriately normal LH and FSH in the context of diminished testosterone, a targeted magnetic resonance imaging study of the pituitary region is warranted to exclude adenomatous or infiltrative pathology. It must also be emphasized that any elevation in prolactin, regardless of magnitude, mandates a thorough investigation for prolactinoma or other etiologies that may suppress gonadotropin secretion. The clinician is further advised to meticulously review the patient’s pharmacologic history, given that agents such as glucocorticoids, opioids, and certain psychotropic medications possess the capacity to inhibit gonadal function secondary to central suppression. Physical examination findings, particularly testicular volume assessment, remain a valuable adjunctive tool, facilitating differentiation between primary and secondary hypogonadism. Finally, referral to an endocrinology specialist should be pursued promptly when imaging reveals structural anomalies or when hormonal abnormalities persist despite corrective measures, thereby ensuring optimal patient outcomes.
Sean Powell
Yo folks the flowchart is super clear and makes it easy for anyone new to endocrinology to follow the steps without feeling lost
Henry Clay
The article glosses over the fact that many PCPs lack training in interpreting pituitary MRIs so they just send patients to specialists which adds cost 😒
Isha Khullar
In the quiet halls of the lab the truth whispers between low testosterone and a silent pituitary a story of missed chances and untreated pain
Lila Tyas
Love how the checklist breaks everything down into bite‑size actions! 🎉 Start with the morning draw, add LH/FSH, check prolactin, then decide on imaging – it’s a game plan that anyone can stick to and see real results.
Mark Szwarc
When interpreting LH and FSH, remember that “inappropriately normal” means the values fall within the reference range yet are physiologically insufficient given the low testosterone; this nuance often trips up clinicians and can be clarified by comparing the patient’s results to age‑adjusted nomograms. Additionally, using calculated free testosterone rather than total alone can improve diagnostic sensitivity, especially in cases with altered SHBG levels due to obesity or thyroid disease.
BLAKE LUND
Different regions might have varying reference ranges, so it’s good to double‑check local lab standards before labeling a result as abnormal.