Venlafaxine Blood Pressure Risk Calculator
How Your Venlafaxine Dose May Affect Your Blood Pressure
This calculator estimates your blood pressure risk based on your current blood pressure reading and venlafaxine dosage. Note: This is for informational purposes only. Always consult your doctor for medical advice.
Enter your values above to see your risk assessment.
When you start taking venlafaxine for depression or anxiety, your doctor likely focuses on whether your mood improves. But there’s another critical change happening inside your body-one that doesn’t always show up in how you feel: blood pressure. Venlafaxine, sold under brands like Effexor and Effexor XR, is one of the most effective antidepressants for people who don’t respond to SSRIs. But it’s also one of the few that can raise your blood pressure, sometimes significantly. This isn’t a rare side effect. It’s a well-documented, dose-dependent risk that demands attention.
How Venlafaxine Raises Blood Pressure
Venlafaxine works by blocking the reabsorption of serotonin and norepinephrine in the brain. That’s why it helps with mood-it keeps these chemicals active longer. But norepinephrine isn’t just a brain chemical. It’s also a key player in your nervous system’s fight-or-flight response. When it builds up in your bloodstream, it tightens blood vessels and makes your heart pump harder. That’s how you get higher blood pressure.
This effect isn’t subtle. At doses below 150 mg per day, the rise in blood pressure is usually small-maybe 1 to 3 mmHg in diastolic pressure. But once you hit 150 mg or more, the norepinephrine effect kicks in hard. Studies show that at doses above 300 mg per day, about 13% of people develop clinically significant hypertension. That’s more than double the rate seen with placebo. Even more concerning, some people develop dangerous spikes in blood pressure at much lower doses. One case report described a 23-year-old man whose blood pressure shot to 210/170 mmHg after just 10 months on 150 mg daily. He had no prior history of high blood pressure.
How It Compares to Other Antidepressants
Not all antidepressants affect blood pressure the same way. SSRIs like sertraline or fluoxetine rarely cause any noticeable rise. Tricyclics like amitriptyline can cause low blood pressure, especially when standing up. But venlafaxine? It consistently pushes blood pressure upward. In head-to-head studies, venlafaxine caused significantly higher blood pressure increases than SSRIs and even some older antidepressants like imipramine.
Desvenlafaxine, the active metabolite of venlafaxine, has similar effects-even at low doses. Duloxetine, another SNRI, tends to have milder effects on blood pressure. That makes venlafaxine stand out: it’s powerful for treatment-resistant depression, but it’s also the SNRI with the clearest link to hypertension.
Who’s at Risk?
You might assume that only people with existing high blood pressure are at risk. That’s not true. In fact, the biggest danger is for people who’ve never had hypertension before. Venlafaxine can push normal blood pressure into the hypertensive range. A 2021 review in Frontiers in Cardiovascular Medicine found that venlafaxine doesn’t worsen preexisting hypertension-it causes new hypertension in people who were previously normal.
That said, if you already have high blood pressure, uncontrolled heart disease, or a history of stroke or heart attack, venlafaxine requires extra caution. Your doctor should check your blood pressure more frequently and consider alternatives. People with kidney disease or those taking other medications that raise blood pressure (like decongestants or stimulants) are also at higher risk.
What the Numbers Really Mean
Let’s put the data in real terms. The FDA says sustained blood pressure elevation is a known risk. The European Medicines Agency notes that while most cases are mild, severe spikes have happened-even at low doses. Here’s what the numbers tell you:
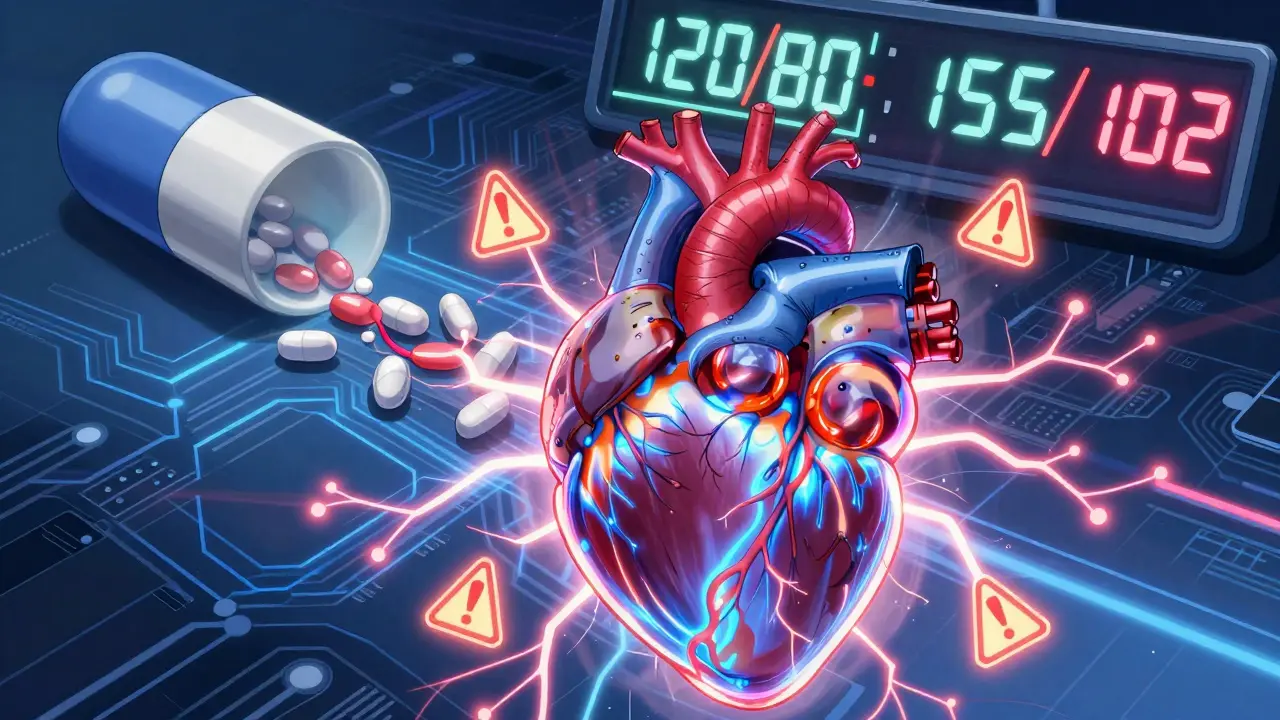
- At doses under 150 mg/day: Blood pressure rise is usually under 3 mmHg diastolic-often not clinically significant.
- At 150-300 mg/day: Risk increases. About 5-8% of people see diastolic pressure rise above 90 mmHg.
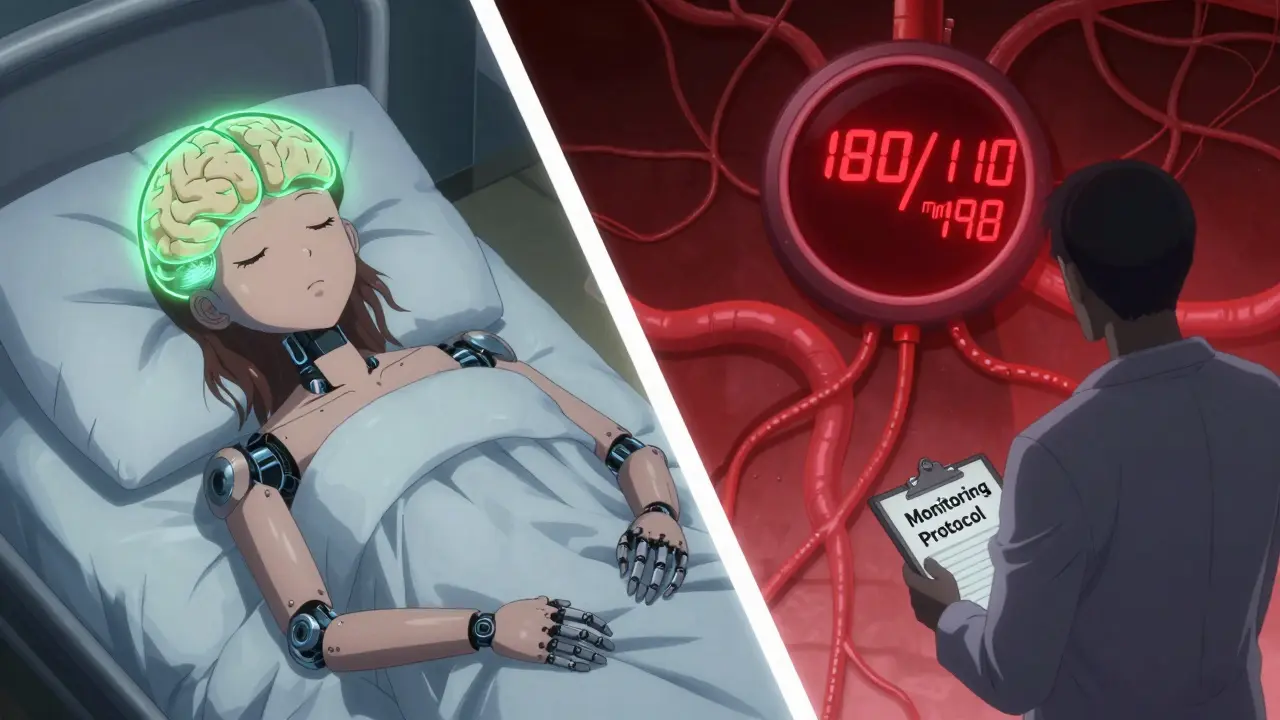
- At doses over 300 mg/day: 13% develop clinically high blood pressure. Some cases reach 180/110 mmHg or higher.
- Even at 37.5 mg/day: Isolated cases of hypertension have been reported. No dose is completely risk-free.
One patient on Reddit reported their blood pressure jumped from 120/80 to 155/102 after two months on 37.5 mg. After stopping venlafaxine, their BP returned to normal in three weeks. That’s not a fluke. It’s a documented pattern.
Monitoring Guidelines: What Your Doctor Should Do
Monitoring isn’t optional. It’s standard care. Here’s what evidence-based guidelines recommend:
- Measure baseline blood pressure before starting venlafaxine.
- Check again at 2 weeks and 4 weeks after starting or increasing the dose.
- For doses above 150 mg/day, monitor monthly for the first 3 months, then every 3 months.
- If blood pressure rises above 140/90 mmHg, reassess the treatment plan.
- If systolic pressure exceeds 180 mmHg or diastolic exceeds 110 mmHg, stop venlafaxine immediately and seek medical help.
The Mayo Clinic and American Psychiatric Association both stress this protocol. Many doctors skip it because patients feel fine. But hypertension from venlafaxine doesn’t cause symptoms until it’s already dangerous. That’s why routine checks matter more than how you feel.
What to Watch For
You might not feel your blood pressure rising. But here are warning signs that could mean trouble:
- Severe, persistent headache
- Nosebleeds (as seen in the 2014 case report)
- Blurred vision or seeing spots
- Chest pain or tightness
- Shortness of breath
- Confusion or dizziness
These aren’t just side effects-they’re red flags for hypertensive crisis. One patient developed posterior reversible encephalopathy syndrome (PRES), a rare but life-threatening brain condition caused by sudden high blood pressure. It’s rare, but it’s been linked to venlafaxine. That’s why ignoring elevated BP isn’t an option.
What Happens If Your Blood Pressure Goes Up?
If your blood pressure rises but stays under 140/90, your doctor might just keep monitoring. If it climbs above that, they’ll likely:
- Lower your dose
- Switch you to a different antidepressant (like an SSRI)
- Add a blood pressure medication if needed
Here’s the good news: in most cases, blood pressure returns to normal within 1 to 4 weeks after stopping venlafaxine. No permanent damage if caught early. But if left unchecked, chronic high blood pressure can lead to heart disease, kidney damage, or stroke.
Real Patient Experiences
On Drugs.com, 28% of negative reviews for venlafaxine mention high blood pressure. On PsychForums, 68% of users reported measurable increases. One user wrote: ‘I started at 75 mg. My BP went from 118/76 to 152/98 in three weeks. My doctor didn’t warn me. I had to bring it up myself.’
But not everyone has the same experience. A patient on PatientsLikeMe with preexisting hypertension said venlafaxine actually helped stabilize their BP fluctuations. That’s rare, but it shows individual variation. Genetics, metabolism, and other medications all play a role.
When Venlafaxine Is Still Worth It
Just because venlafaxine raises blood pressure doesn’t mean you can’t take it. It’s one of the most effective antidepressants for treatment-resistant depression. If SSRIs failed you, venlafaxine might be your best shot at feeling better. The key is managing the risk.
For patients with controlled hypertension, venlafaxine can be used safely-with close monitoring. For those with no history of high blood pressure, starting at a low dose (37.5-75 mg) and checking BP regularly can prevent problems. For older adults or those with heart disease, alternatives like SSRIs or bupropion may be safer.
Global sales of venlafaxine reached $1.2 billion in 2022. Over 23 million prescriptions were filled in the U.S. alone. It’s widely used because it works. But its use must be paired with responsibility-not just from doctors, but from patients too.
Final Takeaway
Venlafaxine is not a ‘safe’ antidepressant just because it’s commonly prescribed. It’s a powerful tool with real cardiovascular risks. The rise in blood pressure isn’t a myth, a rumor, or a rare side effect. It’s a measurable, predictable, and sometimes dangerous effect tied directly to its mechanism of action.
If you’re on venlafaxine, ask your doctor: ‘Have you checked my blood pressure lately?’ If you’re considering starting it, ask: ‘What’s my baseline BP? How often will you check it?’ Don’t wait for symptoms. Don’t assume you’re fine because you feel better mentally. Your body is telling you something else-and ignoring it could cost you more than your mood.
Can venlafaxine cause high blood pressure even at low doses?
Yes. While the risk increases significantly at doses above 150 mg/day, isolated cases of severe hypertension have been reported even at 37.5 mg or 75 mg daily. No dose is completely risk-free. Blood pressure changes can occur without warning, which is why baseline and regular monitoring are essential.
How long does it take for blood pressure to return to normal after stopping venlafaxine?
In most cases, blood pressure returns to baseline within 1 to 4 weeks after discontinuation. The body clears the drug relatively quickly, and the noradrenergic effects fade. However, if hypertension has caused organ damage, recovery may take longer or require additional treatment.
Is venlafaxine safe if I already have high blood pressure?
It can be, but only under close supervision. Studies show venlafaxine doesn’t worsen controlled hypertension in most patients. However, your doctor must ensure your BP is well-managed before starting and monitor it closely. If your blood pressure is uncontrolled (above 140/90), alternatives like SSRIs are usually preferred.
Does switching to Effexor XR reduce the risk of high blood pressure?
No. Both immediate-release and extended-release forms of venlafaxine carry the same risk. The difference is how the drug is absorbed-not how it affects blood pressure. The total daily dose and duration of treatment matter more than the formulation.
Are there antidepressants that don’t raise blood pressure?
Yes. SSRIs like sertraline, escitalopram, and fluoxetine rarely affect blood pressure. Bupropion (Wellbutrin) may slightly lower it in some cases. Mirtazapine and vortioxetine also have minimal cardiovascular effects. These are often safer first choices for people with hypertension or heart disease.
Should I stop venlafaxine if my blood pressure rises?
Don’t stop abruptly. Contact your doctor immediately. If your systolic BP is above 180 or diastolic above 110, seek emergency care. For milder increases (140-179/90-109), your doctor may lower your dose, add a blood pressure medication, or switch you to another antidepressant. Stopping suddenly can cause withdrawal symptoms, so always follow medical guidance.
9 Comments
Juan Reibelo
Just got prescribed venlafaxine last week-150mg. My doctor said, 'You’ll be fine.' I checked my BP yesterday: 148/94. I’m not scared, but I’m not naive either. I’m scheduling a follow-up. If this keeps climbing, I’m switching. No one told me about this risk. Why is it so hidden?
Himanshu Singh
Bro, I was on this for 6 months at 225mg. My BP went from 118/76 to 162/100. I didn’t feel anything. No headaches, no dizziness. Just… felt normal. Then my mom noticed my face looked flushed. She made me check it. 😅 Turned out I was one of those 13%. Stopped it. BP back to normal in 3 weeks. Moral? Don’t wait to feel bad. Check your numbers. 🙏
Jamie Hooper
so like… i was on effexor for anxiety and totally thought it was ‘just me being stressed’ when i kept getting nosebleeds?? like, 3 in one week?? then my roommate was like ‘dude ur bp is wild’ and i was like ‘wait what?’ turns out it was the med. no one warned me. not even the dr. i feel so dumb. but also… why is this not on the box??
Husain Atther
It's important to recognize that while venlafaxine carries a measurable risk, it is not inherently dangerous when used responsibly. The data presented here is comprehensive and should empower patients to engage in informed dialogue with their clinicians. Monitoring is not an inconvenience-it is an act of self-respect. Many of us are conditioned to equate feeling better with being healthy. But mental wellness and cardiovascular health are not mutually exclusive-they must be cultivated together.
Izzy Hadala
Per the FDA Adverse Event Reporting System (FAERS), between 2010 and 2022, there were 1,247 reports of hypertensive emergency associated with venlafaxine use, of which 38% occurred at doses ≤150 mg/day. The median time to onset was 27 days. These are not outliers. This is a pharmacovigilance signal of moderate to high clinical significance. I urge all prescribers to treat this as a class-wide risk, not a rare idiosyncratic reaction.
Elizabeth Cannon
my dr literally said ‘you’re young, you’ll be fine’ when i asked about bp. i’m 29. i’m not invincible. i started checking my bp at home. went from 116/74 to 150/96 in 5 weeks. i’m off it now. and yeah, i cried. but i’m alive. if you’re on this med and you’re not monitoring? you’re playing russian roulette with your heart. stop waiting for symptoms. check your numbers. now.
Phil Maxwell
Yeah, I’ve been on 75mg for 4 months. BP stayed at 122/80. No issues. But I check it every other week. I don’t assume. I don’t ignore. I just… keep an eye. It’s not that scary if you’re paying attention. I’m glad this got posted. More people need to know.
Sushrita Chakraborty
While the pharmacological mechanism is well understood, the clinical implementation remains inconsistent across healthcare systems. In India, where cardiovascular screening is often underprioritized in psychiatric care, this risk is disproportionately under-recognized. Patients are frequently discharged with a prescription and no follow-up protocol. This is not negligence-it is systemic neglect. We must advocate for standardized BP monitoring protocols in psychiatric guidelines globally, not just in Western institutions.
Tommy Sandri
As someone who has worked in mental health clinics across three continents, I can confirm: the disconnect between psychiatric efficacy and somatic monitoring is a global blind spot. Venlafaxine is a gift for treatment-resistant depression-but it is not a benign one. We must normalize BP checks as part of every antidepressant initiation, regardless of age or perceived risk. This isn’t about fear. It’s about integrity in care.