SHPT Treatment Selection Tool
This tool helps determine the most appropriate treatment option for secondary hyperparathyroidism based on key clinical parameters.
Enter patient parameters to receive treatment recommendations
Quick Takeaways
- Secondary Hyperparathyroidism (SHPT) is driven mainly by chronic kidney disease, low vitamin D and high phosphate.
- First‑line drugs are oral calcimimetics (cinacalcet, evocalcet) and active vitamin D analogues (paricalcitol, alfacalcidol).
- New IV calcimimetic etelcalcetide and the selective FGFR‑targeting antibody burosumab are reshaping therapy for dialysis patients.
- Surgical parathyroidectomy remains the most effective option for refractory disease but carries a 5‑10% risk of postoperative hypocalcaemia.
- Regular monitoring of PTH, calcium, phosphate and alkaline phosphatase guides dose adjustments and prevents complications.
What is Secondary Hyperparathyroidism?
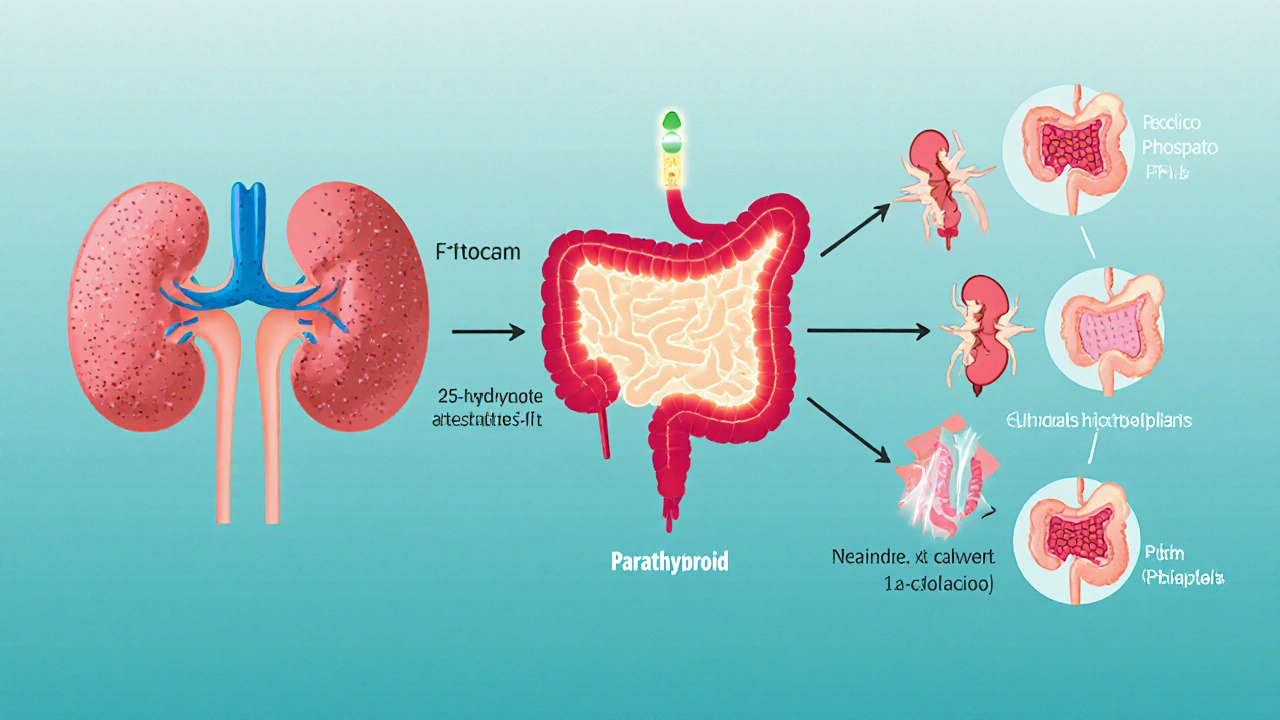
When the kidneys fail to keep mineral balance in check, the parathyroid glands overproduce parathyroid hormone (PTH is a peptide hormone that raises serum calcium and phosphate by acting on bone, kidney and gut.). This compensatory surge is called Secondary Hyperparathyroidism (a disorder where excess PTH arises from another disease, most commonly chronic kidney disease (CKD)). The result is high‑turnover bone disease, vascular calcification and, over time, cardiovascular mortality.
Why does CKD trigger SHPT?
Three inter‑related mechanisms drive the problem:
- Reduced conversion of 25‑hydroxy‑vitamin D to its active form (1,25‑(OH)₂D) lowers calcium absorption from the gut.
- Phosphate retention raises serum phosphate, which directly stimulates PTH secretion.
- Elevated fibroblast growth factor‑23 (FGF23) suppresses vitamin D synthesis and contributes to PTH release.
These disturbances are amplified once patients start dialysis, making early intervention essential.

Diagnosing SHPT
The diagnostic work‑up is straightforward:
- Serum intact PTH: >300 pg/mL in most guidelines for dialysis patients.
- Corrected calcium: keep within 8.4‑10.2 mg/dL.
- Serum phosphate: aim for 3.5‑5.5 mg/dL.
- Bone turnover markers (alkaline phosphatase, bone‑specific alkaline phosphatase) help gauge disease activity.
Imaging (ultrasound, Sestamibi scan) is reserved for surgical planning.
Current Therapeutic Landscape
Guidelines (KDIGO 2023) recommend a three‑pronged approach: control phosphate, suppress PTH, and avoid hypercalcemia.
Phosphate Binders
Calcium‑based binders (calcium acetate, calcium carbonate) are cheap but risk hypercalcemia. Non‑calcium binders (sevelamer, lanthanum) lower phosphate without raising calcium, making them a preferred choice for patients with high calcium‑phosphate product.
Active Vitamin D Analogues
Agents such as paricalcitol and alfacalcidol bind the vitamin D receptor, reducing PTH secretion. They can raise calcium and phosphate, so dosing is titrated carefully.
Calcimimetics
Oral calcimimetics enhance the calcium‑sensing receptor (CaSR) on parathyroid cells, making them think serum calcium is higher than it actually is, which suppresses PTH. The first‑generation agent is cinacalcet; newer agents like evocalcet have smoother dose‑response curves and fewer gastrointestinal side effects.
When Drugs Aren’t Enough: Parathyroidectomy
About 10‑15% of dialysis patients become refractory to medical therapy. In those cases, surgical removal of hyperactive parathyroid tissue (parathyroidectomy) drops PTH by >80% and improves bone pain. The main downside is postoperative hungry bone syndrome, which can drive calcium < 7.0 mg/dL for weeks.
Emerging Therapies Shaping 2025
New drugs target upstream pathways and aim to lessen pill burden.
Etelcalcetide - IV Calcimimetic
Administered at the end of each dialysis session, etelcalcetide binds CaSR via a covalent bond, offering a more predictable PTH reduction. Phase‑III trials (EVOLVE‑2024) showed a 30% greater mean PTH drop versus cinacalcet, with reduced nausea rates.
Selective FGF23 Antagonists
FGF23 neutralising antibodies (e.g., burosumab, though primarily for X‑linked hypophosphatemia) are being repurposed for SHPT. Early‑phase data suggest they restore 1,25‑(OH)₂D levels without increasing phosphate, indirectly lowering PTH.
Small‑Molecule CaSR Allosteric Modulators
Compounds like NPS‑2143 and its derivatives act as positive allosteric modulators but have a longer half‑life, allowing twice‑monthly oral dosing. Ongoing trials (MODULATE‑2025) report comparable PTH control to evocalcet with half the pill count.
Gene‑Therapy Approaches (Experimental)
CRISPR‑based editing of the CaSR gene in parathyroid tissue is still pre‑clinical, but animal models show durable PTH suppression after a single vector delivery. Human trials are slated for 2026.
Choosing the Right Regimen: Decision Framework
Clinicians balance five factors:
- Severity of PTH elevation: >800 pg/mL usually pushes toward combination therapy.
- Calcium‑phosphate product: High product (>55 mg²/dL²) favors non‑calcium binders.
- Dialysis modality: In-centre hemodialysis patients can receive etelcalcetide conveniently.
- Adherence potential: Patients with high pill burden benefit from IV or long‑acting oral agents.
- Risk of surgical complications: Elderly or frail patients may be managed medically longer before considering parathyroidectomy.
Applying this matrix usually leads to one of three pathways:
- Oral calcimimetic + vitamin D analogue for modest PTH levels.
- IV etelcalcetide + phosphate binder for dialysis‑dependent patients with poor oral adherence.
- Parathyroidectomy when PTH >1000 pg/mL despite maximal medical therapy.
Monitoring & Follow‑up
Effective control hinges on regular labs:
| Parameter | Frequency | Target Range |
|---|---|---|
| PTH (intact) | Every 3months | 150‑300pg/mL (dialysis) |
| Corrected Calcium | Monthly | 8.4‑10.2mg/dL |
| Phosphate | Monthly | 3.5‑5.5mg/dL |
| Alkaline Phosphatase | Every 6months | <120U/L (bonespecific) |
If PTH remains above target after 6months of maximally tolerated therapy, consider stepping up to an IV calcimimetic or evaluating surgical candidacy.
Practical Tips & Common Pitfalls
- Don’t chase calcium too low. Over‑suppression can precipitate adynamic bone disease.
- Watch for hypocalcemia with calcimimetics. Calcium carbonate rescue doses work well if symptoms appear.
- Combine phosphate binders wisely. Mixing calcium‑based with non‑calcium binders can lead to unexpected calcium spikes.
- Educate patients on pill timing. Taking calcimimetics with meals improves absorption and limits nausea.
- Plan for postoperative care. After parathyroidectomy, schedule calcium gluconate infusions for the first 24hours and monitor calcium daily for at least a week.
Comparison of Current vs Emerging Therapies
| Therapy | Mechanism | Route | Typical Use | Major Advantage | Common Side‑effects |
|---|---|---|---|---|---|
| Oral calcimimetics (cinacalcet, evocalcet) | CaSR positive allosteric modulator | Oral | Dialysis patients with moderate PTH | Adjustable dose, familiar to patients | Nausea, GI upset, hypocalcemia |
| IV calcimimetic (etelcalcetide) | Covalent CaSR activator | IV (post‑dialysis) | Patients with poor oral adherence | Consistent PTH control, fewer GI issues | Hypocalcemia, infusion site reactions |
| Active vitamin D analogues (paricalcitol, alfacalcidol) | VDR agonist → ↓ PTH synthesis | Oral or IV | Adjunct to calcimimetics | Improves bone mineralization | Hypercalcemia, hyperphosphatemia |
| FGF23 antagonists (experimental) | Neutralises excess FGF23 | Subcutaneous | Refractory SHPT with high FGF23 | Restores vitamin D without raising phosphate | Potential off‑target hormonal effects |
| Parathyroidectomy | Surgical removal of hyperactive glands | Surgical | Severe, refractory SHPT | Rapid, durable PTH reduction | Hungry bone syndrome, recurrent laryngeal nerve injury |
Frequently Asked Questions
What serum PTH level defines secondary hyperparathyroidism in dialysis patients?
Guidelines recommend an intact PTH above 300pg/mL for patients on maintenance hemodialysis, although many clinicians aim for 150‑300pg/mL to balance bone turnover and cardiovascular risk.
When should I consider switching from oral to IV calcimimetic?
If a patient misses more than 20% of oral doses, experiences persistent nausea, or PTH stays >600pg/mL despite maximal oral dosing, etelcalcetide offers more reliable control with fewer GI complaints.
Can vitamin D analogues alone control SHPT?
Alone they modestly lower PTH but often raise calcium and phosphate. Combination with a calcimimetic is the standard to achieve target PTH without overshooting calcium.
What are the signs of hungry bone syndrome after parathyroidectomy?
Rapidly falling calcium (often <7mg/dL), muscle cramps, tingling, and prolonged QT on ECG. Intravenous calcium and vitamin D supplementation are required until bone remineralisation stabilises.
Are there any drug‑drug interactions with calcimimetics?
Cinacalcet is metabolised by CYP3A4; strong inhibitors (ketoconazole, clarithromycin) can raise its levels, increasing hypocalcemia risk. Etelcalcetide is cleared renally and by dialysis, so interaction risk is lower.
14 Comments
charlise webster
Even though KDIGO’s calcium‑phosphate product cutoff gets a lot of hype, clinicians often cherry‑pick the 55 mg²/dL² threshold to justify non‑calcium binders. In reality, many patients sit comfortably below that line and still suffer from vascular calcification because of chronic inflammation. It’s not the product alone; the turnover markers tell you more about bone health than a single lab value. So before you jump on the non‑calcium binder bandwagon, double‑check alkaline phosphatase trends. The guidelines are a starting point, not a rigid rule.
lata Kide
Whoa, the whole “new IV calcimimetic is a miracle cure” narrative feels like a Hollywood trailer 🎬✨! Etelcalcetide might look shiny, but remember the trials still showed a 10‑15 % dropout due to infusion reactions. And the drama doesn’t stop at nausea; we’ve seen spikes in hypocalcemia that could send patients to the ER. If you’re counting pills, sure, dialyzer‑based dosing sounds glamorous, but the reality is a lot of extra nursing time. 🙄💊
Mark Eddinger
The pharmacodynamic profile of evocalcet demonstrates a smoother dose–response curve compared with cinacalcet, which reduces gastrointestinal adverse events. Moreover, the recent phase‑III data indicate a mean PTH reduction of approximately 35 % when titrated to target calcium levels. It is essential to monitor corrected calcium bi‑weekly during the titration phase to avoid overshoot. Clinical judgment should incorporate both laboratory trends and patient‑reported symptoms. This approach aligns with the KDIGO recommendation for individualized therapy.
Francisco Garcia
While the excitement around etelcalcetide is understandable, the practical considerations in a busy dialysis unit matter just as much as efficacy. The need for staff training and the added time at the end of each session can strain resources, especially in smaller centers. Nevertheless, for patients who struggle with oral adherence, the IV route offers a viable alternative. Balancing these factors on a case‑by‑case basis will yield the best outcomes.
Patrick Renneker
The prevailing narrative that newer calcimimetics automatically trump older regimens is overly simplistic.
First, the pharmacoeconomic analyses reveal that etelcalcetide adds a substantial per‑treatment cost that many Medicare‑advantaged populations cannot absorb.
Second, the claim of fewer gastrointestinal side effects overlooks the fact that hypocalcemia–related symptoms, such as paresthesia and muscle cramps, are reported more frequently with the IV formulation.
Third, the convenience argument assumes a well‑staffed dialysis suite, which is far from universal across community programs.
Fourth, the rapid PTH drop can precipitate hungry bone syndrome in a subset of patients.
Fifth, the dose titration algorithm for etelcalcetide is less flexible than the oral alternatives, forcing clinicians into rigid adjustment intervals.
Sixth, the reliance on dialysis access for drug delivery introduces an infection risk that oral agents simply do not carry.
Seventh, patient preference studies indicate that many individuals value oral autonomy over scheduled IV infusions, even if adherence is imperfect.
Eighth, the trial populations were predominantly Caucasian, limiting generalizability to the diverse demographic seen in many US centers.
Ninth, the reduction in PTH, while statistically significant, often falls short of the stringent KDIGO target of 150‑300 pg/mL, necessitating adjunctive therapy.
Tenth, the emphasis on pill burden neglects the broader issue of polypharmacy, where adding another intravenous agent may paradoxically increase overall medication complexity.
Eleventh, the purported smoother dose‑response curve can mask subtle calcium fluctuations that only intensive lab monitoring can uncover.
Twelfth, insurance reimbursement policies lag behind drug approvals, creating a bottleneck that delays patient access.
Thirteenth, the marketing hype surrounding “next‑generation” agents often overshadows the tried‑and‑tested efficacy of established vitamin D analogues when used judiciously.
Fourteenth, clinicians must weigh all these factors before proclaiming any single therapy as the definitive answer.
Finally, a nuanced, patient‑centered algorithm that integrates cost, side‑effect profile, and individual risk factors remains the most prudent path forward.
KAYLEE MCDONALD
Stick to the calcium target; overshoot leads to calciphylaxis.
Alec McCoy
Great points about the hidden costs-remember that every added expense is a chance to empower patients with education, not just a financial hurdle.
Julia C
It’s no coincidence that the pharma lobby rushed these calcimimetics to market right after the Medicare budget cuts; the timing screams a profit‑first agenda disguised as patient‑centered innovation.
Darin Borisov
From a pathophysiological standpoint, the perturbation of the calcium‑sensing receptor cascade by allosteric modulators represents a paradigm shift that necessitates a lexicon beyond conventional nephrology vernacular.
Sean Kemmis
they push new drugs you ignore the old ones but the data is there and it works
Nathan Squire
Oh, brilliant, another “game‑changing” pill-just what we needed after the last breakthrough that turned out to be a placebo in disguise.
satish kumar
Indeed, while the enthusiasm for novel agents is commendable, one must, with due diligence, consider the extensive body of evidence supporting traditional therapies, which, albeit less glamorous, have stood the test of time, and therefore, a balanced appraisal is indispensable.
Kimberly Dierkhising
In practice, the real‑world implementation of these algorithms often collides with workflow bottlenecks, so streamlining the decision tree with clear cutoffs can reduce cognitive load for the care team.
Jessica Forsen
Absolutely, because nothing says “patient‑centric” like a spreadsheet of thresholds that the bedside nurse can memorize during a coffee break.