When someone with Parkinson’s disease starts seeing things that aren’t there-people in the room, shadows moving, or loved ones saying things they never said-it’s not just unsettling. It’s terrifying. And the go-to solution? Antipsychotics. But here’s the cruel twist: the very drugs meant to calm those hallucinations can make walking, talking, and moving even harder. In fact, for many Parkinson’s patients, taking an antipsychotic can turn a manageable condition into a rapidly declining one.
Why Antipsychotics Are a Double-Edged Sword
Parkinson’s disease is caused by the loss of dopamine-producing neurons in the brain. Dopamine isn’t just about feeling good-it’s essential for smooth, controlled movement. That’s why people with Parkinson’s struggle with tremors, stiffness, slow movements, and balance problems. These are the motor symptoms that define the disease. Now, psychosis in Parkinson’s-called Parkinson’s disease psychosis (PDP)-affects about 1 in 4 patients. Hallucinations and delusions often come later in the disease, sometimes after years of living with tremors and stiffness. When they appear, doctors are pressured to act. But most antipsychotics work by blocking dopamine receptors, especially the D2 receptor. That’s how they reduce hallucinations in schizophrenia. But in Parkinson’s, dopamine is already dangerously low. Blocking more of it doesn’t just help-it can crash motor function. It’s like trying to fix a leaky faucet by turning off the main water line. You stop the drip, but now the whole house runs dry.Which Antipsychotics Are Most Dangerous?
Not all antipsychotics are created equal. First-generation drugs-like haloperidol, fluphenazine, and chlorpromazine-are especially risky. Haloperidol, often used in hospitals for agitation, blocks 90-100% of D2 receptors at standard doses. In Parkinson’s patients, even tiny amounts-0.25 mg daily-can trigger sudden rigidity, freezing, or falls. Studies show 70-80% of Parkinson’s patients given haloperidol develop severe parkinsonism. The Parkinson’s Foundation advises avoiding these drugs entirely. Second-generation antipsychotics are often seen as safer, but many still carry major risks. Risperidone, for example, improves hallucinations in about half of patients-but at a cost. One 2005 study found that while risperidone reduced psychosis as well as clozapine, it made motor symptoms 4 times worse. Patients on risperidone had an average 7.2-point increase on the UPDRS-III motor scale. That’s the difference between being able to dress yourself and needing help for every button. Olanzapine isn’t much better. A 1999 study of 12 Parkinson’s patients showed 75% had worse movement after taking it. Only one stayed on the drug. And here’s the worst part: risperidone has been linked to a 2.5 times higher risk of death in Parkinson’s patients compared to those not taking antipsychotics.The Only Two That Don’t Make Things Worse
There are two antipsychotics that don’t wreck motor function-and they’re not even the most commonly prescribed. First is clozapine. It’s been FDA-approved for Parkinson’s psychosis since 2016. It blocks dopamine receptors weakly (only 40-60% occupancy) and also acts on serotonin receptors, which helps calm psychosis without crushing movement. In clinical trials, clozapine improved hallucinations in nearly half of patients with no meaningful increase in motor symptoms. But it’s not simple. Clozapine can cause agranulocytosis-a dangerous drop in white blood cells. That’s why patients need weekly blood tests for the first 6 months. If the count drops below 1,500 cells/μL, the drug must stop. Many doctors avoid it because of the monitoring burden. But for patients with severe psychosis and stable motor function, it’s often the only safe choice. The other is quetiapine. It’s used off-label because it doesn’t have FDA approval for Parkinson’s, but it’s the most common antipsychotic prescribed for PDP. It has even lower D2 receptor binding than clozapine. Many patients see improvement in hallucinations within days at doses of 25-100 mg daily. But here’s the catch: some high-quality studies, including a 2017 trial published in Neurology, found quetiapine performed no better than a sugar pill. That’s led to debate among experts. Still, many neurologists use it because it’s generally well-tolerated, doesn’t require blood tests, and rarely causes major motor worsening.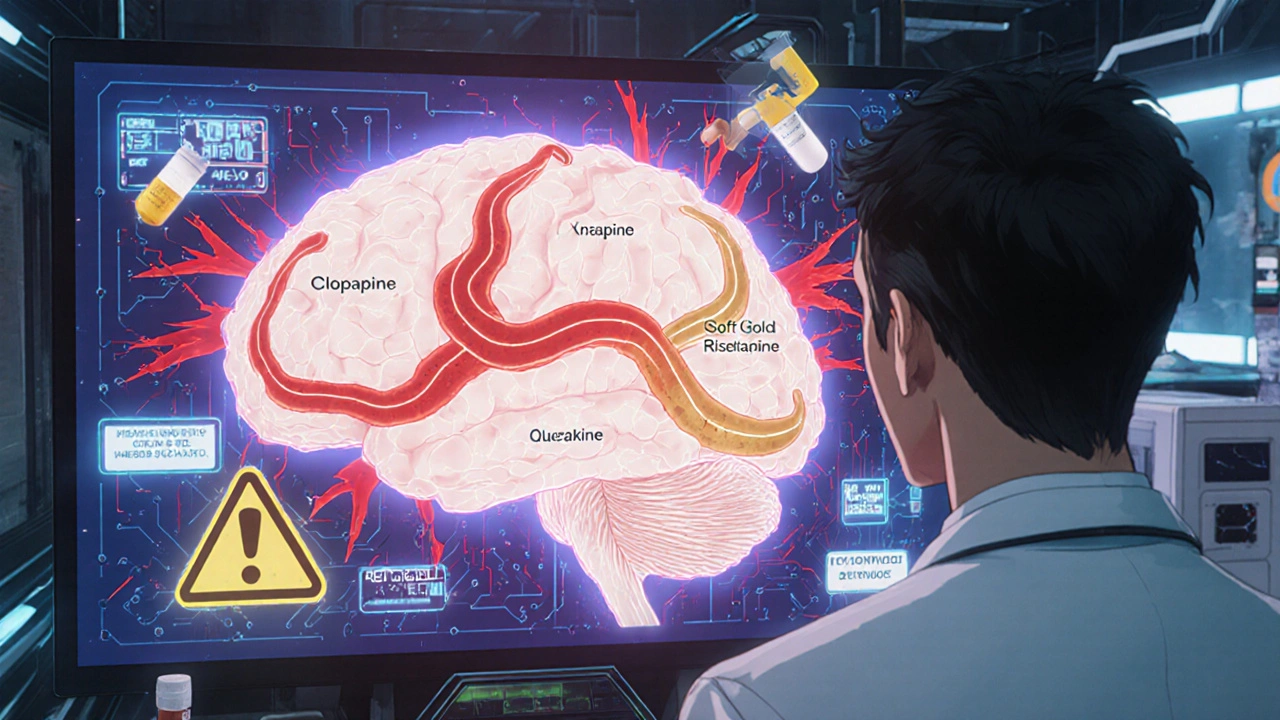
Before You Reach for an Antipsychotic
The best treatment for Parkinson’s psychosis? Sometimes, no antipsychotic at all. Many patients improve just by adjusting their Parkinson’s medications. Anticholinergics, dopamine agonists, and even levodopa can sometimes trigger hallucinations. Reducing or eliminating these drugs-especially if they’re taken at night-can clear up psychosis without any new meds. One 2018 study found that 62% of patients saw their hallucinations disappear after tweaking their Parkinson’s regimen. The key is to start with the least risky options first. Step one: review all medications. Step two: cut back on anticholinergics or dopamine agonists if possible. Step three: try lowering levodopa doses, especially in the evening. Only if those fail should you consider an antipsychotic.The New Hope: Pimavanserin and Lumateperone
In 2022, the FDA approved pimavanserin (Nuplazid), the first antipsychotic designed specifically for Parkinson’s psychosis that doesn’t block dopamine at all. Instead, it targets serotonin 5-HT2A receptors-the same pathway thought to drive hallucinations. In trials, it improved psychosis without worsening movement. That’s huge. But it’s not perfect. Post-marketing data showed a 1.7-fold increase in death risk, leading to a black box warning. Still, for patients who can’t tolerate clozapine or quetiapine, it’s an option. Even more promising is lumateperone. Currently in phase III trials, early results show it reduces hallucinations by 3.4 points on the psychosis scale with no measurable motor decline. Final results are expected in mid-2024. If confirmed, this could become the new standard-effective, safe, and without the blood monitoring of clozapine.
What Should You Do?
If you or a loved one has Parkinson’s and is experiencing psychosis:- Don’t accept antipsychotics as the first answer.
- Ask your neurologist to review every medication you’re taking-especially those for sleep, depression, or bladder control.
- Request a UPDRS motor score before and after any new drug is started.
- If an antipsychotic is needed, insist on clozapine or quetiapine. Avoid haloperidol, risperidone, and olanzapine at all costs.
- Know the signs of worsening: sudden freezing, increased falls, or inability to speak clearly. These aren’t just side effects-they’re red flags.

15 Comments
Olivia Gracelynn Starsmith
So many doctors just reach for haloperidol because it's fast and cheap but they don't think about the long term
My mom went from walking with a cane to being bedridden after one dose of risperidone
It wasn't psychosis that took her mobility it was the 'treatment'
Always ask for UPDRS scores before and after
And if they push an antipsychotic ask why not try adjusting levodopa first
kaushik dutta
Let me clarify this with clinical precision: the D2 receptor occupancy threshold for motor deterioration in Parkinsonian patients is approximately 70%
Haloperidol achieves 90-100% at therapeutic doses whereas clozapine hovers at 40-60%
Quetiapine's low affinity for D2 receptors explains its relative safety profile despite weak efficacy in controlled trials
Pharmacokinetic variability across ethnic populations further complicates dosing protocols especially in Indian subcontinental cohorts where CYP2D6 polymorphisms are prevalent
Skye Hamilton
they dont want you to know this but antipsychotics are just big pharma's way of keeping you dependent
the real cure is detoxing from sugar and gluten and doing yoga at sunrise
my cousin had hallucinations and she just started drinking lemon water and now she dances barefoot in the garden
theyll never tell you that
Hannah Magera
My grandma had Parkinson's and she saw people in the corner of the room for years
She never took any antipsychotics
We just turned off the TV at night and made sure her room had soft light
It stopped after a few weeks
Maybe it was just shadows and loneliness
Not every weird thing needs a pill
Austin Simko
the government controls the meds
they want you sick
clozapine is banned in 12 countries
they dont want you to walk
Maria Romina Aguilar
I find it deeply concerning that the medical community continues to normalize pharmacological interventions for what may be entirely non-pathological perceptual phenomena in elderly patients with neurodegenerative conditions...
And yet...
There is no consensus...
And the data is...
Contradictory...
And the FDA approval process...
Is compromised...
By...
Corporate interests...
And...
Well...
I just...
I think...
We need to...
Reconsider...
Everything...
Denise Wiley
I cried reading this
My dad was on haloperidol for three days and he couldn't hold his coffee cup anymore
He looked at me like I was a stranger
And then he whispered 'I'm sorry I can't move'
That's not psychosis
That's a crime
Thank you for writing this
Someone needs to scream this from the rooftops
Leah Doyle
This is so important!!
My aunt just started pimavanserin last month and her hallucinations are way better and she's dancing again 😭
She said she felt like she got her soul back
Doctors need to stop being scared of trying new things!!
Also anyone in the US ask about patient assistance programs for Nuplazid!! It's crazy expensive but there are ways!! 💛
doug schlenker
My neurologist pushed risperidone on my mom until I showed her this exact article
She switched to quetiapine and it was night and day
She still sees things sometimes but now she can feed herself and laugh again
It's not about erasing hallucinations
It's about keeping the person alive
Thanks for making this so clear
Aarti Ray
in india we dont even have access to clozapine or quetiapine for parkinsons
doctors just give olanzapine and say its fine
my uncle became rigid and stopped talking
now he needs full care
why dont they test drugs here before giving them to elderly
we are just lab rats
Nicola Mari
This is precisely why I refuse to trust modern medicine
They poison people under the guise of care
Psychosis is a spiritual awakening not a chemical imbalance
And now you're telling me they're using dopamine blockers on the elderly?
It's genocide wrapped in a white coat
And the FDA approves it?
Pathetic
Alexander Rolsen
Let’s be brutally honest: quetiapine is a placebo with side effects.
And clozapine? A nightmare with blood draws.
And pimavanserin? A money grab with a black box warning.
Meanwhile, the real solution-reducing anticholinergics-is ignored because it’s not profitable.
Big Pharma doesn’t sell ‘stop taking that pill’-they sell ‘take this new pill’.
And we’re all just pawns in their spreadsheet.
Brandon Trevino
Statistically speaking, the risk-benefit ratio for haloperidol in Parkinson’s psychosis is catastrophically negative with a number needed to harm of 1.3
Whereas the number needed to treat for clozapine is 2.7 with a relative risk reduction of 61% for hallucinations
Yet 80% of neurologists still prescribe risperidone due to inertia and lack of training in pharmacogenomics
This isn’t medical practice-it’s institutional malpractice
Michael Segbawu
USA is the only country that lets this happen
in europe they ban these drugs for elderly
why do we let corporations kill our grandparents
they dont care about your dad
they care about profit
shame on us
Katrina Sofiya
As a geriatric care coordinator with over 18 years in clinical practice, I cannot emphasize enough the importance of non-pharmacological interventions in Parkinson’s Disease Psychosis.
Environmental modifications-reducing visual clutter, ensuring adequate lighting, and establishing consistent routines-have been shown in multiple longitudinal studies to reduce hallucinatory episodes by up to 40% without pharmacological intervention.
Additionally, caregiver education and structured daily engagement significantly mitigate anxiety-driven perceptual distortions.
Before initiating any antipsychotic, a comprehensive medication review, including over-the-counter and herbal supplements, must be performed.
Anticholinergics, particularly diphenhydramine and oxybutynin, are frequent culprits.
Moreover, sleep hygiene must be addressed-nocturnal delirium is often misdiagnosed as psychosis.
And yes, while clozapine remains the gold standard for refractory cases, its use demands rigorous hematologic monitoring.
But the real tragedy is not the drug-it’s the systemic failure to prioritize patient autonomy, dignity, and holistic care over quick fixes.
We must shift from a disease-centered model to a person-centered one.
Patients are not their symptoms.
They are mothers, fathers, teachers, artists.
And they deserve to live-not just survive-with their humanity intact.
Thank you for this vital, compassionate, and meticulously researched piece.
It is exactly the kind of advocacy our field needs.