By age 50, one in three women and one in five men will break a bone because of weak bones. Not from a car crash or a sports injury - but from a simple fall, even just stumbling while getting out of bed. This isn’t normal aging. This is osteoporosis, and it’s silently weakening millions of bones right now.
Most people don’t feel their bones getting brittle. There’s no pain until it’s too late. That’s why waiting for a fracture to happen is like waiting for a leak to flood your house before fixing the pipe. The good news? You can stop it. Not with magic pills, but with clear, proven steps anyone can take - starting today.
Why Your Bones Are Losing Density
Your bones aren’t static. They’re alive, constantly breaking down and rebuilding. Up until your late 20s, your body builds more bone than it breaks down. That’s when you hit your peak bone mass. After that, you slowly lose it - about 0.5% per year. But for women, right after menopause, that loss jumps to 2-3% per year for five to seven years. Men don’t get that sudden drop, but they still lose bone as they age, especially after 70.
It’s not just age. Genetics play a big role. If your mom or dad broke a hip, your risk goes up by 60-80%. Women of White or Asian descent are more likely to develop osteoporosis than Black or Hispanic women. But genetics aren’t destiny. What you do - what you eat, how you move, what you avoid - matters just as much.
The Big Risk Factors You Can Change
Here’s what actually moves the needle on your fracture risk:
- Not enough calcium - Adults need 1,000 mg a day. Over 50? 1,200 mg. Most people get less than half that. Dairy isn’t the only source - fortified plant milks, canned salmon with bones, kale, and tofu made with calcium sulfate all count.
- Vitamin D deficiency - Nearly half of U.S. adults have levels below what’s needed for bone health. Without enough vitamin D, your body can’t absorb calcium, no matter how much you take. Sunlight helps, but in places like Leeds, winter sun isn’t enough. Supplements of 800-1,000 IU daily are often needed.
- Smoking - Just one pack a day increases fracture risk by 55%. Smoking messes with estrogen, reduces blood flow to bones, and makes bone cells less active.
- Drinking too much alcohol - More than two units a day (that’s a bit over one glass of wine) raises hip fracture risk by 41%. Alcohol blocks bone rebuilding and increases fall risk.
- Being inactive - Sitting all day is like telling your bones to stop growing. People who don’t move enough have 25-30% higher fracture risk. Weight-bearing exercise is the only thing that tells your bones: “Stay strong.”
These aren’t vague suggestions. These are measurable, proven drivers of bone loss. Fix one, and your risk drops. Fix two? It drops even more.
What About Medications and Medical Conditions?
Some causes of bone loss aren’t lifestyle-related. Long-term use of corticosteroids - like prednisone for asthma or arthritis - can zap 5-15% of your bone density in just one year. That’s faster than menopause. If you’re on these drugs long-term, talk to your doctor about bone protection.
Other conditions sneak in. Rheumatoid arthritis causes inflammation that attacks bone directly. Type 1 diabetes triples fracture risk. Even type 2 diabetes - which often comes with higher bone density - still increases fracture risk by 40% because bones become brittle in different ways. If you have any of these, don’t assume your bone scan looks fine. You need extra attention.
And here’s the most shocking thing: one fracture makes another much more likely. If you break a vertebra, your chance of breaking another within a year jumps by 86%. Break a hip? Your risk of another fracture skyrockets by 200%. That’s why the first fracture is the biggest red flag - not the bone scan number.
How to Test Your Bone Health
The gold standard is a DXA scan - a quick, low-radiation X-ray of your hip and spine. It takes 15-20 minutes. The radiation? Less than you get from three hours of natural background exposure. Results come as a T-score:
- -1.0 or higher: Normal
- -1.0 to -2.5: Osteopenia (low bone mass)
- -2.5 or lower: Osteoporosis
The U.S. Preventive Services Task Force recommends DXA scans for all women over 65. But if you’re a woman over 50 with risk factors - family history, early menopause, low body weight, smoking - get tested earlier. Men over 70 should also be tested. If you’ve had a fracture after 50, you need one now.
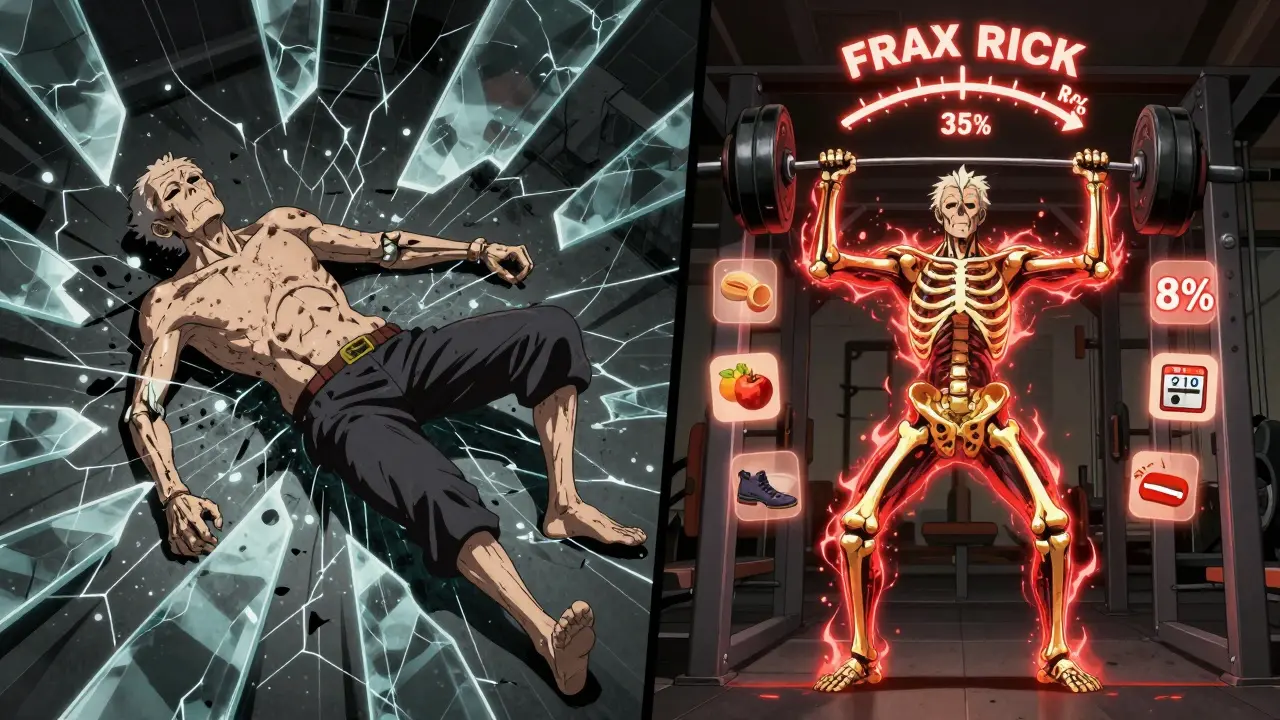
And here’s the catch: bone density alone misses half the people who will fracture. That’s why tools like FRAX are so important. FRAX doesn’t just look at your scan. It adds in your age, weight, smoking status, alcohol use, and whether you’ve had a prior fracture. It gives you a 10-year risk percentage. If it’s over 20%, you’re in the high-risk zone - and you need action.
What Actually Works to Prevent Fractures
Let’s cut through the noise. You don’t need expensive supplements or gimmicks. Here’s what science says works:
- Move your body - Do at least 30 minutes of weight-bearing exercise five days a week. Walk briskly. Climb stairs. Dance. Lift weights twice a week. You don’t need to run a marathon. Just keep loading your bones. Studies show this cuts fracture risk by 30-40%.
- Get the right nutrients - Aim for 1,000-1,200 mg of calcium daily. Split it into two doses - your body can only absorb 500-600 mg at once. Pair it with 800-1,000 IU of vitamin D. If you’re deficient, you may need 2,000 IU daily for a few months to catch up.
- Stop smoking - Quitting cuts your fracture risk by 30% within five years. Even cutting back helps.
- Limit alcohol - Stick to one drink a day. Less is better.
- Prevent falls - Remove tripping hazards at home. Install grab bars in the bathroom. Get your vision checked. Do balance exercises like standing on one foot for 30 seconds, twice a day. The CDC’s STEADI program shows this reduces falls by nearly 30%.
Exercise isn’t optional. It’s the most powerful bone-strengthening tool you have. A 2022 study with over 2,500 people found that those who stuck with a supervised exercise program for six months improved their balance by 45% and cut their falls in half.
What Doesn’t Work - And What to Avoid
Many people try supplements without checking their levels first. Taking extra calcium when you’re not deficient? It won’t help - and might even harm your heart. Same with mega-doses of vitamin D. More isn’t better. Stick to the recommended amounts.
Also, don’t wait for pain. If you’re losing height, developing a hunched back, or having back pain without injury - those are signs of vertebral fractures. Get checked. Don’t assume it’s just “getting older.”
And avoid the myth that “I’m too old to start.” People in their 80s who begin weight-bearing exercise still gain bone density. It’s never too late to strengthen what’s left.
The Bigger Picture
Osteoporosis isn’t just about bones. It’s about independence. A hip fracture can end your ability to live alone. One in five people who break a hip die within a year. Many never walk again. The cost? Over $57 billion a year in the U.S. alone.
But prevention pays off. Every dollar spent on bone health saves $5.40 in future fracture care. That’s why the best time to act was years ago. The second best time? Today.
Start with one change. Get your vitamin D level checked. Walk 20 minutes a day. Talk to your doctor about a DXA scan if you’re over 50 with risk factors. Don’t wait for a fall to wake you up. Your bones are counting on you - and you’re stronger than you think.
Can you reverse osteoporosis naturally?
You can’t fully reverse osteoporosis, but you can stop it from getting worse - and even rebuild some bone. Weight-bearing exercise, enough calcium and vitamin D, and quitting smoking can improve bone density over time. Some medications, like romosozumab, can rebuild bone quickly, but they’re only for high-risk patients. The goal isn’t to return to your 20s - it’s to stay strong enough to avoid fractures.
Is walking enough for bone health?
Walking helps, but it’s not enough on its own. You need to challenge your bones with impact and resistance. Brisk walking, stair climbing, and dancing are good. Add strength training twice a week - squats, lunges, resistance bands - to really stimulate bone growth. Walking keeps you mobile; adding resistance builds strength.
Do I need a bone density scan if I feel fine?
Yes - if you’re a woman over 65, a man over 70, or anyone over 50 with risk factors like a family history of hip fracture, smoking, or long-term steroid use. Osteoporosis has no symptoms until you break a bone. A scan takes 20 minutes. A fracture can change your life forever. Don’t wait for pain to act.
What’s the best calcium supplement?
Calcium citrate is better absorbed on an empty stomach and works well for people with low stomach acid. Calcium carbonate is cheaper and needs to be taken with food. Either is fine if you take the right dose (500-600 mg at a time) and split it into two doses daily. Avoid coral or bone meal supplements - they may contain lead. Look for third-party tested brands with USP or NSF labels.
Can vitamin D alone prevent fractures?
No. Vitamin D helps your body absorb calcium, but it doesn’t build bone by itself. You need both. And you need movement. Studies show vitamin D alone reduces fracture risk only slightly. When combined with calcium and exercise, the effect is strong. Don’t rely on one thing. Build a full strategy.

8 Comments
pradnya paramita
Per the ISCD guidelines, bone mineral density (BMD) assessment via DXA is the gold standard for diagnosing osteoporosis, with T-scores below -2.5 indicating disease. However, FRAX integrates clinical risk factors beyond BMD-like glucocorticoid use, prior fracture, and low BMI-to generate 10-year fracture probability. For patients with osteopenia (-1.0 to -2.5) and FRAX >20%, pharmacologic intervention (e.g., bisphosphonates or denosumab) is indicated even without a prior fracture. Bone turnover markers (CTX, P1NP) can also monitor treatment response.
Roshan Gudhe
It’s funny how we treat bones like they’re just scaffolding. They’re alive. They breathe. They remember. You think it’s about calcium pills and walking? Nah. It’s about showing up for your body every single day-not because you’re scared of breaking, but because you still believe you’re worth holding together. 🌱
Wendy Lamb
Just got my DXA scan. T-score of -2.1. Osteopenia. Started walking daily and took vitamin D3. No supplements yet. Waiting for my doctor’s advice.
Antwonette Robinson
Oh wow, another article telling me I’m dying because I didn’t drink enough milk in 1998. Next they’ll say my posture is the reason the dinosaurs went extinct.
caroline hernandez
As a physical therapist who’s worked with geriatric patients for 18 years, I can tell you the single most effective intervention isn’t calcium or vitamin D-it’s progressive resistance training. Two days a week, 3 sets of 8-12 reps with controlled eccentric loading on squats, step-ups, and seated rows. That’s what triggers osteoblast activity. No magic. Just mechanics. And yes, I’ve seen 82-year-olds gain 4% BMD in 9 months. It’s not about age. It’s about stimulus.
Justin Fauth
My grandpa broke his hip at 76. He never walked again. We didn’t do anything. We just said ‘he’s old.’ That’s not American. That’s giving up. We don’t quit on our bodies. We lift weights, we take our vitamins, we walk. If you’re not doing something for your bones by 50, you’re already behind. Get off the couch. America doesn’t have time for weak bones.
Meenal Khurana
Thank you for the clear info. I’ll talk to my doctor about the scan.
Joy Johnston
Thank you for this comprehensive, evidence-based overview. I’d like to add that recent meta-analyses (e.g., BMJ 2023) confirm that combined calcium + vitamin D supplementation reduces non-vertebral fracture risk by 14% in high-risk populations, but only when adherence exceeds 80%. Also, for patients on proton-pump inhibitors, calcium citrate is preferred due to reduced gastric acid dependency. Consistency > intensity. And please-avoid the trendy ‘bone broth’ supplements. They’re not clinically validated.