Myocardial Ischemia Symptom Checker
Symptom Assessment Result
Did you know that about 1 in 4 heart attacks start with a silent episode of myocardial ischemia that many people overlook?
Quick Takeaways
- Typical symptoms include chest pressure, shortness of breath, and unexplained fatigue.
- Diagnosis relies on ECG, stress testing, cardiac biomarkers, and sometimes coronary angiography.
- Treatment ranges from medication (beta‑blockers, nitrates) to procedures like PCI or CABG, plus lifestyle changes.
- Immediate medical attention is crucial if pain spreads to the arm, jaw, or is accompanied by sweating.
- Long‑term management focuses on risk‑factor control and regular follow‑up.
What Is Myocardial Ischemia?
Myocardial Ischemia is a condition where the heart muscle receives insufficient blood flow, usually because of narrowed or blocked coronary arteries. The reduced oxygen supply can cause chest discomfort, limit exercise tolerance, and, if untreated, lead to a heart attack.
It is often considered a precursor to Coronary Artery Disease, the broader term for any damage or blockage in the coronary vessels.
How to Spot the Symptoms
Symptoms vary widely, and some people experience no pain at all. Recognizing the subtle cues can prevent a full‑blown infarction.
- Chest pressure, heaviness, or squeezing that lasts a few minutes.
- Shortness of breath, especially during exertion or when lying flat.
- Unexplained fatigue or weakness, even after light activity.
- Upper‑body discomfort - pain or tingling in the shoulders, arms, neck, jaw, or back.
- Nausea, cold sweats, or light‑headedness without a clear cause.
When symptoms appear at rest, worsen at night, or are accompanied by vomiting, treat them as an emergency.
How Doctors Diagnose Myocardial Ischemia
The diagnostic pathway blends patient history with a series of tests that reveal how the heart responds to stress and whether blood flow is compromised.
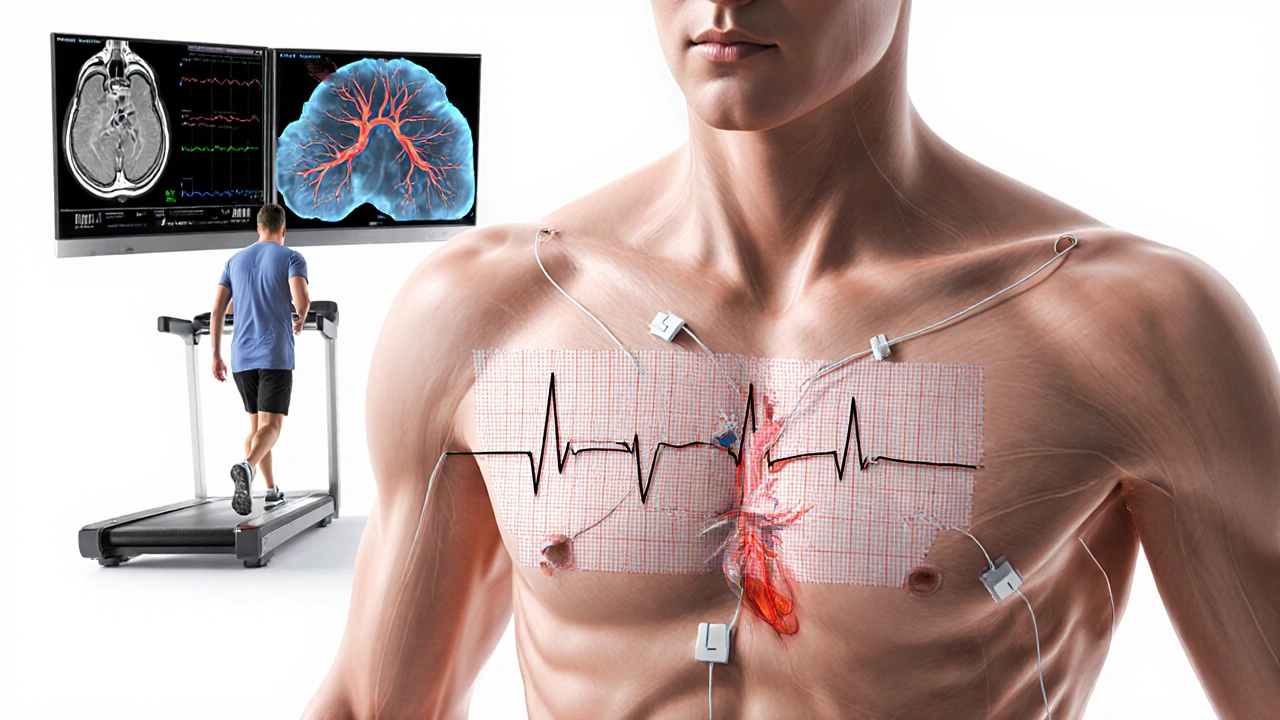
Electrocardiogram (ECG)
Electrocardiogram records the heart’s electrical activity. Specific changes-ST‑segment depression or T‑wave inversion-can flag ischemia even when the patient feels fine.
Stress Testing
A Stress Test pushes the heart to work harder, usually on a treadmill or stationary bike, while monitoring ECG and blood pressure. The test reveals hidden blockages that only appear under load.
Cardiac Biomarkers
Blood tests for troponin, CK‑MB, and myoglobin assess heart‑muscle injury. In early ischemia, troponin may be slightly elevated, indicating ongoing damage.
Imaging Techniques
- Echocardiography: Ultrasound evaluates heart motion; regional wall‑motion abnormalities suggest reduced blood flow.
- Cardiac MRI: Provides detailed tissue characterization and can quantify the size of ischemic zones.
Coronary Angiography
When non‑invasive tests point to significant blockage, doctors may perform Coronary Angiography. A contrast dye visualizes the arteries under X‑ray, allowing precise measurement of narrowing.
Treatment Options Explained
Managing myocardial ischemia involves three layers: medication, revascularization procedures, and lifestyle modification.
Medication
First‑line drugs aim to reduce heart workload, improve oxygen delivery, and prevent clot formation.
- Beta‑Blockers lower heart rate and contractility, cutting oxygen demand.
- Nitrates dilate coronary vessels, relieving chest discomfort.
- Antiplatelet agents (e.g., aspirin, clopidogrel) reduce platelet aggregation, lowering the risk of clot‑related blockage.
Revascularization
When medication isn’t enough, restoring blood flow directly becomes necessary.
- Percutaneous Coronary Intervention (PCI) involves threading a balloon‑tipped catheter to open the artery and often placing a stent.
- Coronary Artery Bypass Grafting (CABG) is open‑heart surgery that creates new routes for blood using vein or arterial grafts.
Lifestyle Changes
Even after medical therapy, risk‑factor control is vital.
- Quit smoking - reduces coronary spasm and plaque buildup.
- Adopt a Mediterranean‑style diet rich in fruits, vegetables, whole grains, and oily fish.
- Engage in at least 150 minutes of moderate aerobic exercise per week, as tolerated.
- Manage hypertension and diabetes through medication and regular monitoring.
Comparing Treatment Paths
| Aspect | Medication | PCI | CABG |
|---|---|---|---|
| Invasiveness | Non‑invasive | Minimally invasive (catheter‑based) | Highly invasive (open‑heart) |
| Recovery time | Days to weeks | 1‑2 weeks | 4‑8 weeks |
| Effectiveness for single‑vessel disease | Symptom relief, limited | High success (90%+) | Reserved for multi‑vessel or left‑main disease |
| Long‑term patency (vessel staying open) | Depends on disease progression | Stent restenosis ~5‑10% | Graft durability 10‑15 years (arterial) |
| Typical candidates | Stable angina, low‑risk patients | Persistent symptoms despite meds, suitable anatomy | Complex disease, diabetes, left‑main blockage |

Living with Myocardial Ischemia
After diagnosis, ongoing self‑monitoring matters more than any single test.
- Keep a symptom diary - note what triggers chest pressure and how long it lasts.
- Schedule regular follow‑up appointments; repeat stress tests every 1‑2 years if risk remains high.
- Use a home blood‑pressure cuff and, if prescribed, a portable ECG device for early detection.
Embrace a heart‑healthy routine: balanced meals, consistent sleep (7‑8 hours), and stress‑relief practices such as mindfulness or light jogging.
When to Call Emergency Services
Even if you’ve been told you have “stable” ischemia, certain warning signs demand immediate care.
- Chest pain that radiates to the left arm, jaw, or back and lasts longer than 5 minutes.
- Sudden, severe shortness of breath with sweating or nausea.
- Loss of consciousness or a feeling of impending faint.
Dial 999 (UK) or your local emergency number without delay.
Frequently Asked Questions
Can myocardial ischemia be completely cured?
It can often be controlled and its progression halted, especially when risk factors are aggressively managed. In many cases, revascularization (PCI or CABG) restores normal blood flow, but lifelong lifestyle habits and medication remain essential.
Is chest pain always a sign of myocardial ischemia?
No. Chest discomfort can stem from acid reflux, muscle strain, or anxiety. However, any new, unexplained chest pressure should be evaluated by a clinician to rule out cardiac causes.
What lifestyle changes give the biggest benefit?
Quitting smoking, adopting a Mediterranean‑style diet, and regular aerobic exercise each cut the risk of progression by roughly 20‑30% according to recent cardiology studies.
How often should I get a stress test?
If you have stable disease and no new symptoms, every 1‑2 years is typical. Your doctor may recommend more frequent testing if risk factors worsen.
Are there any new drugs on the horizon?
Recent trials show promise for PCSK9 inhibitors and novel anti‑inflammatory agents that further reduce plaque buildup, but they are currently prescribed for high‑risk patients under specialist guidance.

17 Comments
April Rios
When we contemplate myocardial ischemia, we are forced to confront the fragile balance between supply and demand that defines the very essence of cardiac physiology. The heart, a relentless engine, demands a constant stream of oxygenated blood, yet the insidious narrowing of coronary vessels can tip this equilibrium into peril. Symptoms, though variable, serve as cryptic whispers from the myocardium, urging us to listen before the silence of a full infarction settles in. Chest pressure, the most iconic herald, may masquerade as mere indigestion, reminding us that perception is often clouded by routine. Shortness of breath, especially when it erupts at rest, signals that the heart is struggling to meet metabolic needs even in the absence of exertion. Fatigue, that lingering exhaustion, can be the body's subtle protest against chronic under‑perfusion. The physician's toolbox-ECG, stress testing, biomarkers, and imaging-acts as a series of lanterns illuminating hidden territories of ischemia. An ST‑segment depression on a resting ECG is a subtle scar, while an exercise‑induced T‑wave inversion can unmask latent compromise. Biomarkers such as troponin, though traditionally markers of necrosis, may rise modestly in the setting of prolonged ischemia, offering a biochemical clue. Imaging modalities, from echocardiography to cardiac MRI, provide visual confirmation of wall‑motion abnormalities or perfusion deficits. Treatment, therefore, must be tiered: lifestyle modification, pharmacotherapy, and when anatomy dictates, revascularization through PCI or CABG. Beta‑blockers and nitrates can reduce myocardial oxygen demand, buying precious time for the heart to recover. Antiplatelet agents prevent the final act of clot formation that would otherwise seal the fate of the myocardium. While revascularization restores flow, it does not absolve the patient from the lifelong stewardship of risk factors. Quitting smoking, embracing a Mediterranean diet, and engaging in regular aerobic activity are the humble yet powerful allies in this battle. Ultimately, myocardial ischemia reminds us that vigilance, early recognition, and a multifaceted therapeutic approach are the pillars upon which survivorship rests.
byron thierry
From a clinical perspective, the presentation of myocardial ischemia can be deceptively subtle, therefore a high index of suspicion is warranted. The integration of patient history with objective data such as electrocardiographic changes provides a robust diagnostic framework. It is essential to recognize that symptom variability does not diminish the underlying pathophysiology. Prompt referral for stress testing or coronary angiography when indicated can alter the trajectory of disease progression.
bob zika
Indeed, the contemporary guidelines, which emphasize risk stratification, recommend a multi‑modal assessment, including biomarkers, imaging, and functional testing; moreover, the clinician must consider comorbid conditions, such as diabetes and hypertension, which exacerbate ischemic burden; consequently, therapeutic decisions should be individualized, aligning with patient preferences and evidence‑based protocols.
M Black
Yo, if you feel that tight chest thing just chill a bit and call 911 if it sticks 😎 stay safe out there
Sidney Wachira
Behold! The heart, that stubborn tyrant, unleashes its fire‑brand pain, a drama worthy of the gods themselves! ⚡️ Yet many wander blind, dismissing the flare as mere indigestion, oblivious to the ticking doom that lurks beneath! 🎭 Hear the warning, dear traveler, before the curtain falls! 🌟
Aditya Satria
Understanding myocardial ischemia begins with acknowledging the balance between oxygen demand and supply; when that balance is disturbed, the heart signals distress. Early identification through diligent monitoring can prevent catastrophic outcomes. Patients are encouraged to adopt heart‑healthy habits, as lifestyle modifications profoundly influence disease trajectory. Moreover, evidence‑based therapies, when applied promptly, can restore perfusion and improve quality of life. Stay hopeful, because modern medicine offers robust tools to combat this condition.
Jocelyn Hansen
Great job on learning the basics!, now let’s dive a little deeper, shall we?; remember, the key to managing ischemia lies in both medical therapy and lifestyle changes, and you’ve got this! 😊 Keep tracking symptoms, stay active, and never hesitate to ask your doctor about any concerns, because prevention is power!
Joanne Myers
The clinical course of myocardial ischemia demands a nuanced approach, integrating pharmacologic therapy with procedural interventions. Patient education remains paramount, ensuring adherence to treatment regimens.
rahul s
Yo bro, think of your heart as a busted highway-traffic jams of blood cause epic jams, and you gotta clear that road fast. Drop the smokes, feast on greens, and let your ticker run like a racehorse on steroids (the healthy kind). Keep it lit, keep it moving.
Julie Sook-Man Chan
I always double‑check my chest pain triggers.
Amanda Mooney
Regular follow‑ups are essential for monitoring disease progression. Early detection of changes can guide timely interventions.
Mandie Scrivens
Sure, because ignoring chest pain always works out great. Let's not try that again.
Natasha Beynon
Monitoring your blood pressure at home can catch early signs of worsening ischemia. Combine this with a balanced diet for optimal heart health. Consistency is the secret.
Cinder Rothschild
When considering the broader sociocultural context of cardiovascular health one cannot overlook the pervasive influence of dietary patterns that have been shaped over centuries by migration, trade routes and industrialization; the modern Western diet, rich in saturated fats and refined sugars, stands in stark contrast to traditional plant‑based cuisines that historically dominated many regions, providing a cornucopia of antioxidants and fiber that protect vascular integrity; epidemiological studies consistently demonstrate lower incidence of myocardial ischemia among populations adhering to such diets, suggesting a profound interplay between cultural food practices and cardiac outcomes; therefore public health initiatives must not only address individual behavior change but also strive to reshape collective culinary narratives, promoting accessibility to wholesome foods while mitigating socioeconomic barriers that perpetuate unhealthy choices; clinicians, too, have a role in educating patients about these macro‑level influences, encouraging small, sustainable modifications that align with cultural preferences and personal tastes, thereby fostering adherence and long‑term cardiovascular benefit.
Oscar Brown
In the grand tapestry of human physiology, the heart occupies a central, almost mythic, position, beating ceaselessly as the metronome of life itself; yet, within this seemingly invincible organ, lies a vulnerability dictated by the laws of fluid dynamics and atherosclerotic progression, a paradox that physicians have endeavored to unravel for centuries; myocardial ischemia, as a manifestation of this paradox, presents itself not merely as a clinical entity but as a reminder of the delicate equilibrium between vascular patency and myocardial demand, a balance that is perpetually threatened by modifiable and immutable risk factors; contemporary diagnostic modalities, ranging from electrocardiographic interpretation to sophisticated cardiac magnetic resonance imaging, afford us unprecedented insight into the ischemic substrate, enabling stratified therapeutic strategies that encompass pharmacologic agents, percutaneous interventions, and surgical revascularization; nevertheless, the ultimate arbiter of outcome remains the patient's commitment to lifestyle alteration, adherence to medication, and vigilant monitoring, underscoring the synergistic relationship between medical science and patient agency; thus, it is incumbent upon the medical community to not only treat the physiological derangements but also to cultivate an environment wherein preventative measures are accessible, culturally resonant, and sustainably implemented, for therein lies the true potential to attenuate the burden of myocardial ischemia upon society.
Tommy Mains
Take your meds as prescribed and keep an eye on any new chest discomfort. If something feels off, call your doctor right away. Staying proactive can make all the difference.
Alex Feseto
The contemporary discourse surrounding myocardial ischemia often suffers from a paucity of rigorous scholarly engagement, thereby necessitating a reexamination of prevailing pedagogical doctrines; one must aspire to elevate the caliber of discussion, invoking a synthesis of empirical evidence and theoretical acumen that befits the gravitas of cardiovascular pathology.