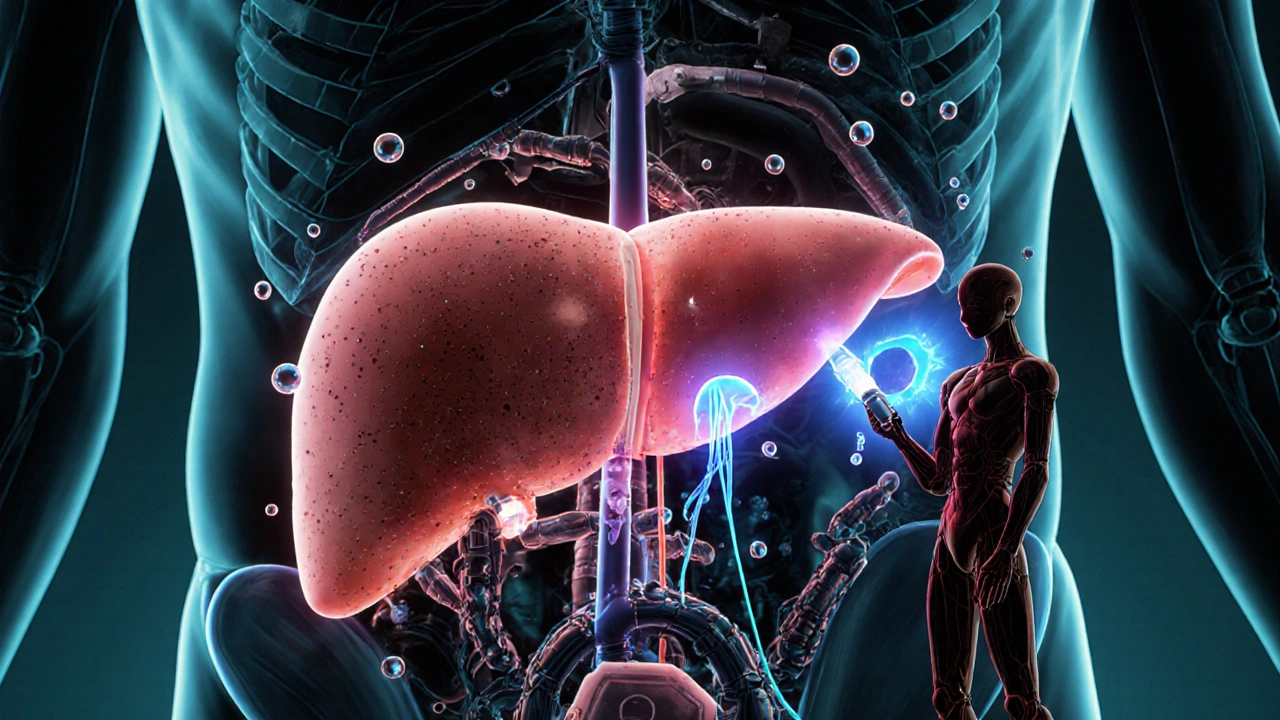
More than 1 in 4 adults worldwide have fat building up in their liver-not from drinking alcohol, but from metabolic problems. This isn’t just a minor issue. Left unchecked, it can lead to inflammation, scarring, and even liver failure. The condition used to be called NAFLD, but since 2023, experts now call it MASLD-Metabolic Dysfunction-Associated Steatotic Liver Disease. The name change matters because it shifts the focus from what’s not causing the problem (alcohol) to what is-obesity, insulin resistance, high blood sugar, and belly fat. And the good news? You can reverse it. Not with a magic pill, but with real, sustained weight loss-and in many cases, GLP-1 receptor agonists.
What Exactly Is MASLD?
MASLD isn’t just ‘a little fatty liver.’ It’s defined by fat making up more than 5% of your liver cells, plus at least one metabolic issue: being overweight (BMI 30+), having type 2 diabetes, high blood pressure, or abnormal cholesterol. The liver isn’t just storing fat-it’s struggling to process it. About 20% of people with MASLD develop MASH, the more serious form with liver inflammation and damage. Left alone, 20-30% of those with MASH will develop cirrhosis over 10 to 15 years. That’s why catching it early matters.
Why does fat build up? Three main reasons: your body sends too many fatty acids from fat tissue to your liver (that’s 59% of the problem), your liver makes its own fat from sugar and carbs (26%), and your liver doesn’t burn fat or ship it out efficiently. It’s a perfect storm of metabolic dysfunction.
Weight Loss Isn’t Optional-It’s the Foundation
If you do nothing else, losing weight is the single most effective way to improve MASLD. But not just any weight loss. Studies show you need to lose at least 5-7% of your body weight to reduce liver fat. That’s 10-15 pounds for someone who weighs 200. But if you want to actually reverse inflammation and scarring, you need to hit 10% or more.
The Look AHEAD trial proved this: people who lost 10% of their weight cut their risk of developing MASH by 90% compared to those who didn’t. How? Losing weight reduces the flood of fatty acids from your belly fat into your liver. It also cuts down on how much fat your liver makes from sugar-by 25-35%. And it helps your liver burn fat better.
Experts recommend aiming for 7-10% weight loss over 6 to 12 months. That means eating 1,200 to 1,800 calories a day (depending on your size), moving at least 150 minutes a week (brisk walking counts), and focusing on whole foods-vegetables, lean protein, healthy fats, and complex carbs. Cut out sugary drinks, refined carbs, and processed snacks. The Mediterranean diet works best here. It’s not a fad. It’s the most studied and proven approach.
GLP-1 Drugs: The Game Changer
What if you’ve tried diet and exercise but can’t lose that last 10%? Or you have type 2 diabetes and your blood sugar won’t budge? That’s where GLP-1 receptor agonists come in. These are injectable medications like semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda). They were originally made for diabetes and obesity, but now they’re being used to treat MASLD too.
Semaglutide, at 2.4 mg per week, helped people lose an average of 15% of their body weight in clinical trials. In one study, 55% of MASLD patients saw their liver fat cut in half. Liraglutide helped 39% of patients reverse MASH-compared to just 17% on placebo. The mechanism? These drugs improve insulin sensitivity, reduce fat production in the liver, and lower inflammation by blocking key signals like NF-κB.
One of the most compelling studies, the REGENERATE trial, showed that semaglutide 1.0 mg (the diabetes dose) led to MASH resolution in 52% of patients after 72 weeks. That’s more than double the placebo group. And it wasn’t just about weight loss-the drug had direct effects on liver tissue.

Combining Weight Loss and GLP-1 Drugs Works Best
Doctors aren’t saying, ‘Take the shot and eat whatever you want.’ The real power comes from combining both. GLP-1 drugs make it easier to lose weight and keep it off. They reduce hunger, slow stomach emptying, and help you feel full longer. That’s huge for people who’ve struggled with dieting for years.
Real-world data shows that when patients get GLP-1 drugs and structured dietary support, 65% stick with treatment after a year. Without counseling, adherence drops to 42%. That’s the difference between success and failure. A patient in the MASLD Patient Registry lost 12.3% of their weight on semaglutide and saw their liver fat score drop from 328 to 245 on FibroScan-a clear sign of improvement.
But it’s not a cure-all. GLP-1 drugs don’t fix advanced scarring (F3-F4 fibrosis). If your liver is already heavily scarred, you might need other treatments, like resmetirom, which is expected to be approved soon. Also, about 30-40% of people stop GLP-1 drugs because of nausea, vomiting, or diarrhea. That’s why starting low and going slow matters. Many doctors start at 0.25 mg per week and increase over 16-20 weeks.
What You Need to Know Before Starting
Before you jump on a GLP-1 drug, get tested. You need to know your liver fat level and fibrosis stage. Tools like FibroScan (a painless ultrasound) and MRI-PDFF give accurate readings. Your doctor should also calculate your FIB-4 score-a simple blood test that estimates liver scarring.
Cost is a real barrier. Semaglutide runs about $1,350 a month. Liraglutide is close behind at $1,250. Medicare covers about two-thirds of patients for obesity, but private insurance varies. Some patients use patient assistance programs from manufacturers. And don’t assume it’s covered for MASLD alone-it’s often only approved for obesity or diabetes.
Side effects are common but manageable. Nausea is the biggest issue. Many doctors prescribe pyridoxine (vitamin B6) at 25 mg twice a day to help. Eating smaller meals, avoiding greasy foods, and staying hydrated helps too. Most side effects fade after 4-6 weeks.

What Happens If You Stop?
This is the hard truth: if you stop the medication, you’ll likely regain the weight-and the fat will come back to your liver. Studies show that 42% of people regain more than half their lost weight within two years after stopping. That’s why long-term management is key. Think of GLP-1 drugs like blood pressure meds-not a quick fix, but a tool to help you rebuild your health.
Some patients eventually taper off after reaching their goals and maintaining them with lifestyle changes. But for many, especially those with type 2 diabetes or severe obesity, it’s a long-term treatment. The goal isn’t just to lose weight-it’s to protect your liver for life.
Where Things Are Headed
The MASLD market is exploding. It’s projected to hit $28 billion by 2030. New drugs like tirzepatide (Mounjaro) are showing even better weight loss than semaglutide. Resmetirom, the first drug approved specifically for MASH, could soon be combined with GLP-1 drugs for even better results.
But access is uneven. While 72% of U.S. academic hospitals now have MASLD clinics, only 28% of rural counties have specialists. If you’re in a small town, you might need to travel or rely on telehealth. Don’t wait. Start with your primary care doctor. Ask for a liver ultrasound or FibroScan. Get your blood sugar and cholesterol checked. And if you’re overweight or diabetic, don’t ignore your liver.
MASLD is silent until it’s serious. But it’s also one of the few chronic liver diseases you can reverse-with the right tools, the right support, and the right commitment. Weight loss isn’t easy. GLP-1 drugs aren’t perfect. But together, they’re changing the game.
Can you reverse MASLD without medication?
Yes, but only if you lose enough weight. Losing 5-7% of your body weight reduces liver fat. Losing 10% or more can reverse inflammation and even fibrosis in many cases. The key is consistency-most people regain weight without ongoing support. Diet, exercise, and behavior change are the foundation. Medication helps when lifestyle alone isn’t enough.
How long does it take to see liver improvement with GLP-1 drugs?
Liver fat starts dropping within weeks, but meaningful improvement-like reduced inflammation or fibrosis-takes 6 to 12 months. In the REGENERATE trial, patients saw the best results at 72 weeks (about 18 months). Regular monitoring with FibroScan or MRI-PDFF helps track progress.
Are GLP-1 drugs safe for people with liver disease?
Yes, they’re generally safe. GLP-1 drugs are metabolized by the kidneys, not the liver, so they don’t add stress to a fatty liver. In fact, they help. However, if you have advanced cirrhosis, your doctor will monitor you closely. Rare side effects like pancreatitis or gallbladder issues can occur, but these are uncommon. Always get tested before starting.
Do I need a liver biopsy to diagnose MASLD?
No. Biopsies are rarely needed anymore. Non-invasive tests like FibroScan (for fat and stiffness) and blood tests like FIB-4 or ELF score are now the standard. MRI-PDFF is the most accurate for measuring liver fat. Biopsies are only used if the results are unclear or if advanced fibrosis is suspected.
Can I take GLP-1 drugs if I don’t have diabetes?
Yes. Semaglutide (Wegovy) and liraglutide (Saxenda) are FDA-approved for chronic weight management in people without diabetes. If you have MASLD and obesity, you can qualify even if your blood sugar is normal. Your doctor will check your BMI, liver tests, and metabolic markers to determine eligibility.
What’s the difference between MASLD and MASH?
MASLD is the umbrella term for fatty liver caused by metabolic dysfunction. MASH (Metabolic Dysfunction-Associated Steatohepatitis) is the more serious form-it means there’s inflammation and liver cell damage in addition to fat buildup. MASH carries a higher risk of cirrhosis and liver cancer. Not everyone with MASLD has MASH, but everyone with MASH has MASLD.
9 Comments
Paige Lund
So basically, if I just stop eating bread, my liver magically fixes itself? Cool, I’ll get right on that.
Frank Dahlmeyer
Look, I’ve been fighting this for years-trying keto, intermittent fasting, even that weird seaweed cleanse my cousin swore by-and nothing worked until I started semaglutide. I lost 22% of my body weight in a year, my FibroScan went from 380 to 190, and my doctor said my liver looks like a 30-year-old’s. But here’s the kicker-it didn’t happen because I ‘got motivated.’ It happened because the drug rewired my hunger signals. I stopped craving sugar like it was oxygen. I didn’t ‘try harder.’ I got help. And if you’re sitting there judging people who use GLP-1s, you haven’t tried to lose weight after 40 with insulin resistance. You just don’t know what you’re talking about.
Dion Hetemi
Let’s be real-this whole MASLD thing is just Big Pharma’s new cash cow. GLP-1 drugs cost $1,300 a month? That’s a luxury tax on the working class. Meanwhile, the same people pushing these drugs are telling you to ‘just eat less and move more’ like it’s 1998. The system’s rigged. You need money to fix a disease caused by poverty, processed food, and lack of access to healthcare. This isn’t science-it’s capitalism with a liver ultrasound.
Christopher Robinson
Just wanted to add a real-world note: I’m a nurse in rural Ohio, and we’ve started referring all obese patients with elevated liver enzymes for FibroScan. No biopsy needed. We’ve had 12 patients start GLP-1s with dietary coaching through telehealth. Eight of them are still on it after 8 months. Two dropped out due to nausea (we titrated slower next time), three lost 10%+ and reversed early MASH. One guy’s FIB-4 dropped from 2.8 to 0.9. It’s not magic, but it’s working where lifestyle alone failed. Don’t write it off-just make sure you’re getting the right support.
harenee hanapi
Oh wow, another article telling people with fatty liver to ‘lose weight’ like it’s a moral failure. Meanwhile, the same people who wrote this are probably sipping matcha lattes in their Silicon Valley offices while millions of Americans can’t afford fresh vegetables. You talk about ‘reversing’ MASLD like it’s a Netflix documentary. Have you ever tried eating clean when your paycheck ends on the 15th and the only grocery store within 20 miles sells Doritos and canned spam? This isn’t about discipline-it’s about systemic neglect. And now you want to charge $1,300/month for a drug that makes you puke? Thanks, capitalism.
James Ó Nuanáin
As a British medical historian with a PhD in hepatology from Oxford, I must express my profound dismay at the casual misrepresentation of metabolic pathology in this piece. The term ‘MASLD’ was formally adopted by the European Association for the Study of the Liver in 2023 following rigorous consensus criteria-not some marketing committee. Furthermore, the assertion that ‘weight loss reverses fibrosis’ is misleading; only early-stage fibrosis (F1-F2) demonstrates significant regression, and even then, only with sustained ≥10% weight loss over 18–24 months. The REGENERATE trial’s 52% MASH resolution rate was achieved under controlled conditions with weekly clinical monitoring-not in the real world where 60% of patients discontinue GLP-1s within 6 months due to gastrointestinal intolerance. To suggest this is a ‘game changer’ without acknowledging adherence rates and socioeconomic barriers is not only scientifically irresponsible-it is ethically negligent.
river weiss
I’ve been a primary care provider for 22 years. I’ve seen patients lose 50 pounds on GLP-1s and regain it all in 6 months after stopping. I’ve seen others lose 20 pounds with diet and exercise alone and keep it off for 7 years. The truth? There’s no single answer. What works is personal. What matters is access-access to nutritionists, access to affordable meds, access to mental health support. I don’t care if you use Ozempic or just cut soda. What I care about is whether you’re being heard. If your doctor dismisses you because you’re ‘just overweight,’ find a new one. Your liver doesn’t care about your BMI number-it cares about your next meal, your sleep, your stress levels, and whether you feel like you can change. This isn’t a drug story. It’s a humanity story.
Kara Binning
So let me get this straight-you’re telling me that if I’m fat and have a fatty liver, I’m basically a lazy, irresponsible person who just needs to eat less? And if I can’t do it, I should pay $1,300 a month for a drug that makes me throw up? Meanwhile, my neighbor’s kid eats nothing but chicken nuggets and Sprite and has a liver that looks like a newborn’s. Hmm. Interesting. I’ll stick with my 2000-calorie-a-day diet and my emotional eating. At least I’m not paying for a pill to fix my trauma.
Codie Wagers
There’s a deeper metaphysical truth here: MASLD isn’t a disease of the liver-it’s a disease of the soul’s relationship with consumption. We live in a culture of instant gratification, where food is comfort, and discomfort is an enemy to be medicated. The GLP-1 drugs don’t cure fat-they force a confrontation with the void we’ve been stuffing with carbs. The real reversal isn’t in the liver cells-it’s in the surrender to discipline, to patience, to the quiet courage of choosing broccoli over bread. The body follows the mind. And if your mind is still screaming for sugar, no drug, no matter how expensive, will ever heal you. You must become the person who doesn’t need the drug. That’s the real therapy.