When your kidneys aren't working right, taking the same pills you always have can be dangerous. It’s not just about taking less-it’s about knowing which drugs to avoid, when to change the dose, and how to spot trouble before it’s too late. For millions with chronic kidney disease (CKD), medication errors are one of the leading causes of hospital visits. A 2022 study found that nearly 24% of prescriptions for CKD patients were given at unsafe doses. That’s not a small mistake. That’s a preventable crisis.
Why Kidneys Matter More Than You Think
Your kidneys don’t just make urine. They filter your blood. Every pill you swallow-whether it’s for blood pressure, diabetes, or a headache-passes through them. If your kidneys are damaged, those drugs stick around too long. That’s when side effects turn into emergencies: high potassium, low blood pressure, or even kidney failure from something as simple as an ibuprofen tablet. The key number doctors use is eGFR-estimated glomerular filtration rate. It tells you how well your kidneys are filtering. Normal is above 90 mL/min/1.73 m². Once it drops below 60, you’re in stage 3 CKD. Below 30? That’s stage 4. And below 15? You’re in stage 5-kidney failure. Each drop means your body handles drugs differently.Drugs That Can Hurt Your Kidneys (Nephrotoxins)
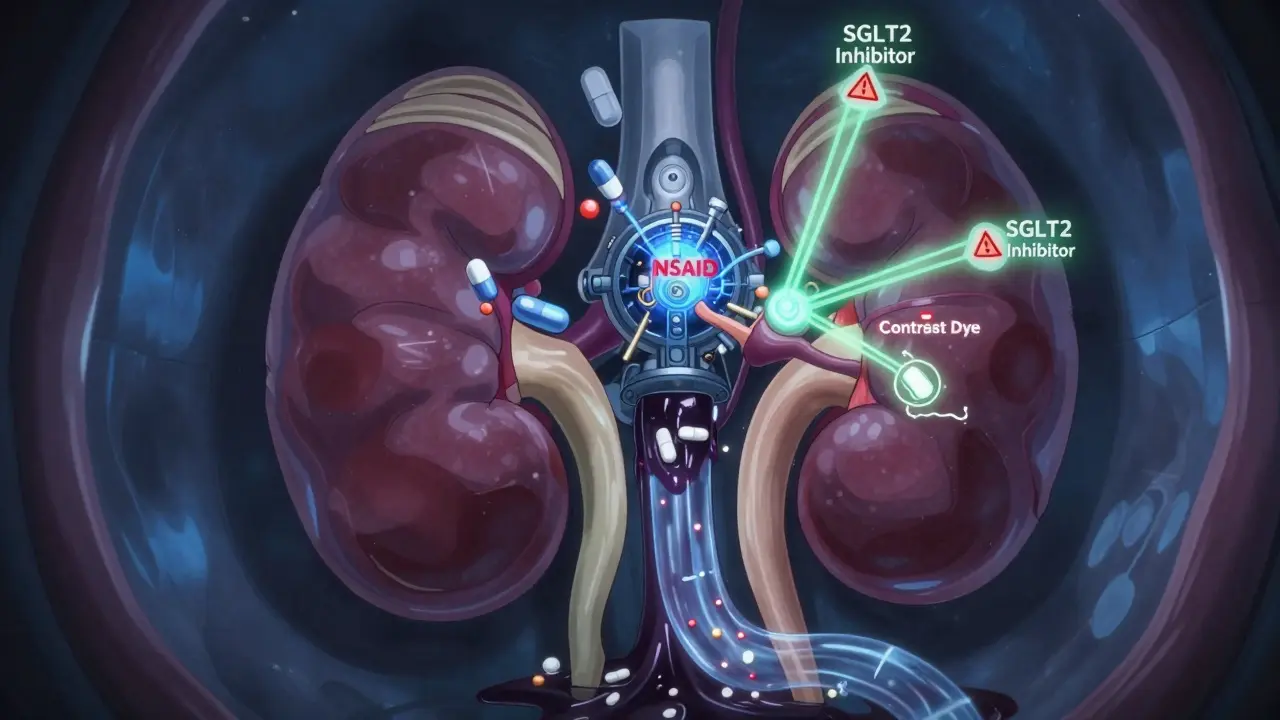
Some medications are like sandpaper on your kidneys. They don’t just need dose changes-they need to be avoided entirely.- NSAIDs (ibuprofen, naproxen, diclofenac): These are the biggest offenders. A single dose can trigger acute kidney injury in someone with CKD. One patient on Reddit shared how two Advil spiked his creatinine from 3.2 to 5.7 in 48 hours. He ended up in the ER.
- Sodium phosphate bowel prep: Used before colonoscopies, this can cause severe kidney damage. Alternatives like polyethylene glycol (PEG) are safer and now recommended by the DoD/VA in their 2025 guidelines.
- Aminoglycosides (gentamicin, tobramycin): Antibiotics used for serious infections. They’re hard on kidneys. Dosing must be adjusted to once daily instead of every 8 hours when eGFR is under 60.
- Contrast dye: Used in CT scans. Can cause contrast-induced nephropathy. Hydration and timing matter-but many hospitals still skip proper screening.
When to Adjust Doses-The eGFR Rules
Not all drugs need to be stopped. Many just need lower doses or longer gaps between doses. Here’s what the latest KDIGO 2024 guidelines say:- eGFR 60-89: Usually no change needed for most drugs. Still monitor.
- eGFR 30-59: Start adjusting. Many antibiotics, diuretics, and pain meds need lower doses.
- eGFR 15-29: High risk. Doses must be cut significantly. Some drugs need to be avoided entirely.
- eGFR under 15: No dialysis? This is the hardest zone. Dosing is guesswork without therapeutic drug monitoring (like checking vancomycin levels in your blood).
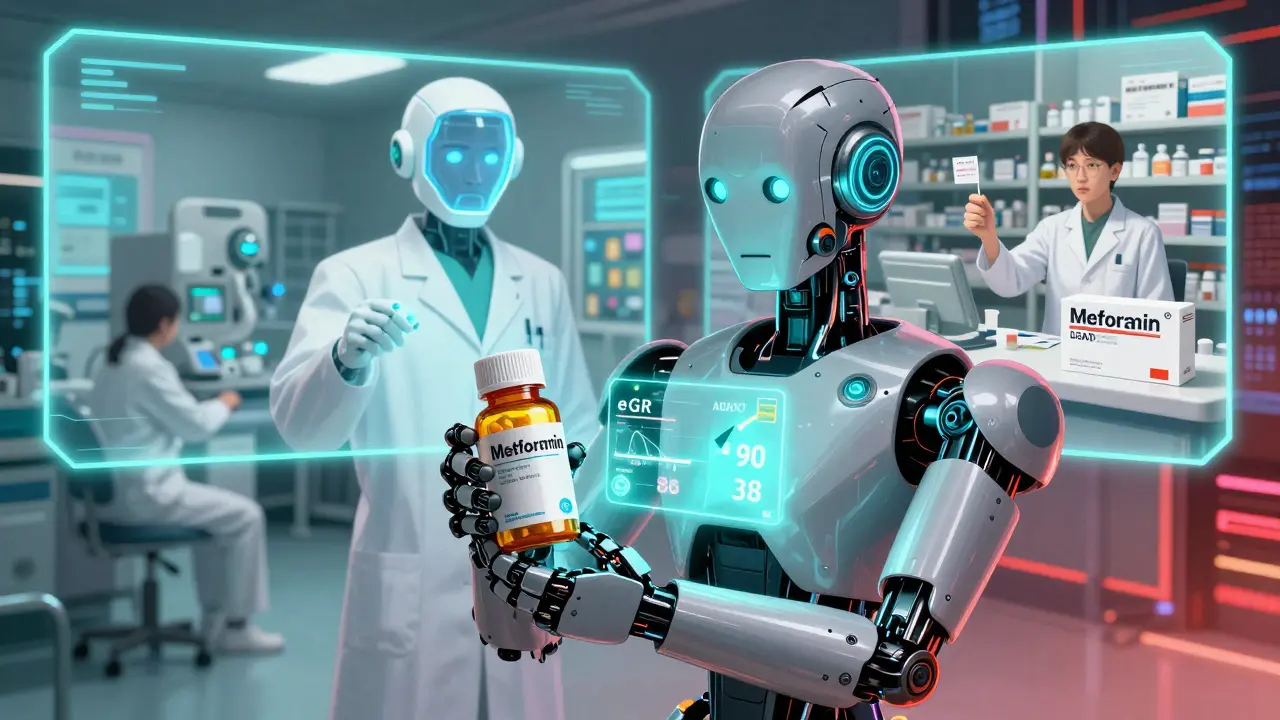
Diabetes Medications: A Game-Changer
If you have diabetes and CKD, your medication choices matter even more. Older drugs like metformin used to be off-limits at eGFR below 60. Now? The rules changed.- Metformin: Safe down to eGFR 30. Avoid if below 30. The risk of lactic acidosis is real but rare if you’re not sick or dehydrated.
- Sulfonylureas (glipizide, glyburide): Avoid. They cause dangerous low blood sugar in kidney patients.
- SGLT2 inhibitors (dapagliflozin, empagliflozin): These are the breakthrough. They work the same at eGFR 10 as they do at 90. No dose adjustment needed. Studies show they cut the risk of kidney failure by 39%. They’re now recommended even if you don’t have diabetes.
- GLP-1 agonists (semaglutide, liraglutide): Also safe in CKD. Help with weight and heart protection.
ACE Inhibitors and ARBs: Don’t Hold Back
For years, doctors avoided these drugs in CKD because they raised creatinine. That was a mistake. KDIGO 2024 says: Maximize the dose. Even if your creatinine goes up 30%, don’t stop. That rise doesn’t mean harm-it means the drug is working. These drugs protect your kidneys by lowering pressure inside the filtering units. Stopping them early means faster decline. And if you still have high albumin in your urine after using the highest tolerated ACE or ARB? Add finerenone. It’s a new drug, approved in 2022, proven to cut kidney failure risk by another 23%.What You Should Do Right Now
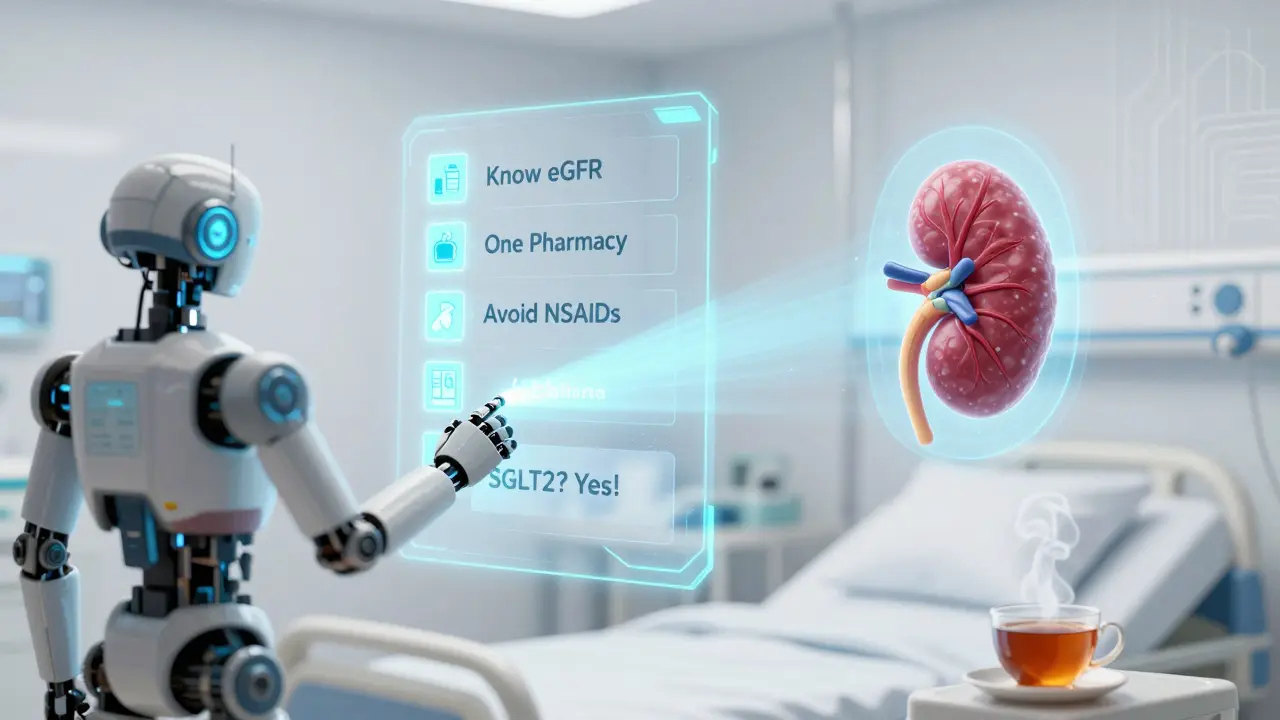
You don’t need to memorize every drug guideline. But you do need a system.- Know your eGFR. Ask for it at every visit. Write it down.
- Keep one pharmacy. Pharmacists can flag dangerous interactions. NIDDK found a 42% drop in kidney injuries when patients used just one pharmacy.
- Review your meds every 3 months. Ask: “Is this still safe for my kidneys?”
- Never take NSAIDs without asking your doctor-even if they’re “over the counter.”
- Ask if your diabetes meds are SGLT2 inhibitors. If not, ask why.
Tools That Help
You’re not alone. There are tools to make this easier:- Epocrates Renal Dosing: Used by 63% of U.S. nephrologists. Free app. Type in a drug and your eGFR-it tells you the dose.
- KDIGO checklist: Some clinics now use printed or digital checklists during visits. One patient said it caught her metformin dose when her eGFR dropped to 38. Saved her from lactic acidosis.
- VA Health System alerts: Since 2019, their EHR system blocks unsafe doses. Result? 37% fewer errors.
What’s Coming Next
The future of kidney-safe prescribing is here. In 2026, the FDA will update its guidelines using real-world data from electronic health records. That means better, faster, smarter dosing rules. Pharmacogenomics-testing your genes to see how you metabolize drugs-is being studied in 17 trials right now. Imagine knowing, before you take a pill, if your body will struggle to clear it because of your kidney disease and your DNA. And KDIGO is rolling out a standardized medication safety checklist for all CKD patients by mid-2026. It’ll be simple: one page, one review, one question: “Are your meds safe for your kidneys today?”Final Thought: Your Kidneys Can’t Speak. You Have To.
Medication safety in kidney disease isn’t about being perfect. It’s about being aware. It’s about asking the right questions. It’s about knowing that a headache pill could cost you your kidneys-and that there’s a safer way. You’re not just managing a disease. You’re protecting your future. And that starts with one conversation-with your doctor, your pharmacist, or even just yourself: “Is this still safe?”Can I still take ibuprofen if I have kidney disease?
No. Ibuprofen and other NSAIDs can cause sudden kidney injury in people with CKD-even if you’ve taken them for years. A single dose can spike creatinine levels and lead to hospitalization. Use acetaminophen (Tylenol) instead for pain, and always check with your doctor before taking any OTC medicine.
What’s the safest diabetes medication for kidney disease?
SGLT2 inhibitors like dapagliflozin and empagliflozin are the safest and most protective. They don’t need dose changes, even with very low kidney function, and they reduce the risk of kidney failure and heart disease. GLP-1 agonists like semaglutide are also excellent choices. Avoid sulfonylureas-they cause dangerous low blood sugar.
Why do some doctors say to stop ACE inhibitors if creatinine rises?
That’s outdated thinking. A rise in creatinine (up to 30%) while on an ACE inhibitor or ARB doesn’t mean the drug is hurting your kidneys-it means it’s working. Stopping it early increases your risk of kidney failure. KDIGO 2024 calls this suboptimal care. Keep the dose unless creatinine rises over 30% and you have symptoms like dizziness or low blood pressure.
How often should I get my kidney meds reviewed?
At least every 3 months if you have stage 3 or worse CKD. More often if you’re sick, hospitalized, or your eGFR changes quickly. A 2023 study showed that primary care providers need about 20 hours of training to get dosing right-so don’t assume your doctor knows all the rules. Ask for a medication review.
Can I take vitamins or supplements with kidney disease?
Many can be harmful. Avoid high-dose vitamin C (can cause oxalate kidney stones), vitamin D without supervision (can raise calcium), and herbal supplements like St. John’s Wort or licorice root-they interfere with kidney meds. Always tell your doctor what you’re taking, even if it’s “natural.”
What should I do before a CT scan or colonoscopy?
For CT scans: Ask if contrast dye is necessary. If yes, request hydration before and after, and avoid if your eGFR is below 30. For colonoscopy: Insist on PEG-based bowel prep (like MiraLAX), not sodium phosphate (Fleet Phospho-soda)-the latter can cause acute kidney injury. Many hospitals still use the unsafe option unless you ask.
Is it safe to take antibiotics if I have kidney disease?
Some are, some aren’t. Aminoglycosides (gentamicin) and vancomycin need dose adjustments. Penicillins and cephalosporins are usually safe but may still need lower doses. Always tell your prescriber your eGFR. Use Epocrates or ask your pharmacist to check. Never take leftover antibiotics without confirmation.
Can I use over-the-counter kidney support supplements?
Avoid them. There’s no proven benefit, and many contain hidden ingredients like aristolochic acid or heavy metals that damage kidneys. The NIDDK warns that 68% of CKD patients are confused about OTC safety. Stick to evidence-based treatments-your doctor, not a bottle on a shelf, should guide your care.
11 Comments
innocent massawe
This is so important. I had no idea ibuprofen could wreck my kidneys so fast. I've been taking it for years for back pain... guess I'm switching to Tylenol now. 🙏
veronica guillen giles
Oh wow. So the doctor who told me to 'just cut back' on NSAIDs was basically giving me a death sentence with a smile? Thanks for the reality check. 🙄
Ian Ring
I appreciate the clarity here. But I must say: the fact that hospitals still use sodium phosphate prep... it's alarming. And yet, they don't even screen eGFR before the procedure? This isn't negligence-it's systemic failure. 😔
Kerry Howarth
SGLT2 inhibitors are game-changers. No dose adjustments. Kidney protection. Heart benefits. If your doctor isn't prescribing these for CKD + diabetes, ask why. Simple.
Joy F
Let’s be real: this isn’t about dosing. It’s about a healthcare system that treats kidneys like disposable filters. We optimize insulin, we monitor cholesterol, but when your GFR drops below 60, suddenly you’re a statistical footnote. And now they want us to ‘ask questions’? Like the doctor who’s already burned out? The system is broken. The guidelines are perfect. The implementation? A dumpster fire. 🗑️
Haley Parizo
You know what’s wild? The same people who scream about pharmaceutical greed are silent when it comes to nephrotoxins. They’ll boycott Big Pharma for a $100 pill... but will pop Advil like candy because it’s ‘over the counter.’ The hypocrisy is breathtaking. This isn’t about medicine-it’s about cultural ignorance.
Ian Detrick
I’ve been living with CKD for 8 years. I used to think ‘watching my meds’ meant avoiding salt. Turns out, it’s about knowing which pills are quiet killers. This post saved me from a hospital trip last month. Thank you.
Angela Fisher
I’ve been reading this and I’m scared. Like, really scared. I’ve been taking those kidney support supplements from Amazon. The ones with ‘natural herbs’ and ‘ancient healing.’ What if they’re secretly poisoning me? What if my doctor doesn’t even know what’s in them? And what if the FDA is hiding this? I think this is all part of a larger cover-up. They don’t want us to know how dangerous our meds really are. I’ve started keeping a journal. I’m not alone in this.
Neela Sharma
In India, we call this ‘dil se dawa’-medicine from the heart. But here? It’s just checkboxes and algorithms. I’m a nurse. I’ve seen elders take NSAIDs for arthritis because the pharmacy didn’t flag it. No one asked. No one cared. This post? It’s not just information. It’s a lifeline. Thank you for speaking truth with care.
Michael Burgess
Just used Epocrates for the first time after reading this. Typed in ‘metformin’ + my eGFR 34. It said ‘safe, no adjustment.’ I cried. My PCP told me to stop it last year. I’ve been off it for 11 months. I feel like a ghost. Now I’m calling my doctor tomorrow. 🙏
Liam Tanner
I’m the author of this post. Thank you all for your thoughtful replies. I didn’t expect this kind of response. The most important thing isn’t the guidelines-it’s that you’re asking. Keep asking. Keep checking. You’re not just managing a disease-you’re claiming your health.