When you’re on Medicaid, getting your prescriptions filled shouldn’t feel like a maze. But for many, it is. Medicaid covers prescription drugs for over 85 million Americans in 2026 - that’s more than one in four people in the U.S. But what drugs are actually covered? How much do you pay? And why does it change from state to state? The answer isn’t simple. It depends on where you live, what drug you need, and whether your doctor jumps through the right hoops.
Medicaid Must Cover Prescriptions - But States Decide Which Ones
Federal law doesn’t force states to cover prescription drugs under Medicaid. Sounds strange, right? But here’s the twist: every single state does cover them anyway. Why? Because without drug coverage, people skip doses, end up in the ER, and cost the system more in the long run. So all 50 states and D.C. offer outpatient prescription drug benefits to nearly all Medicaid enrollees.
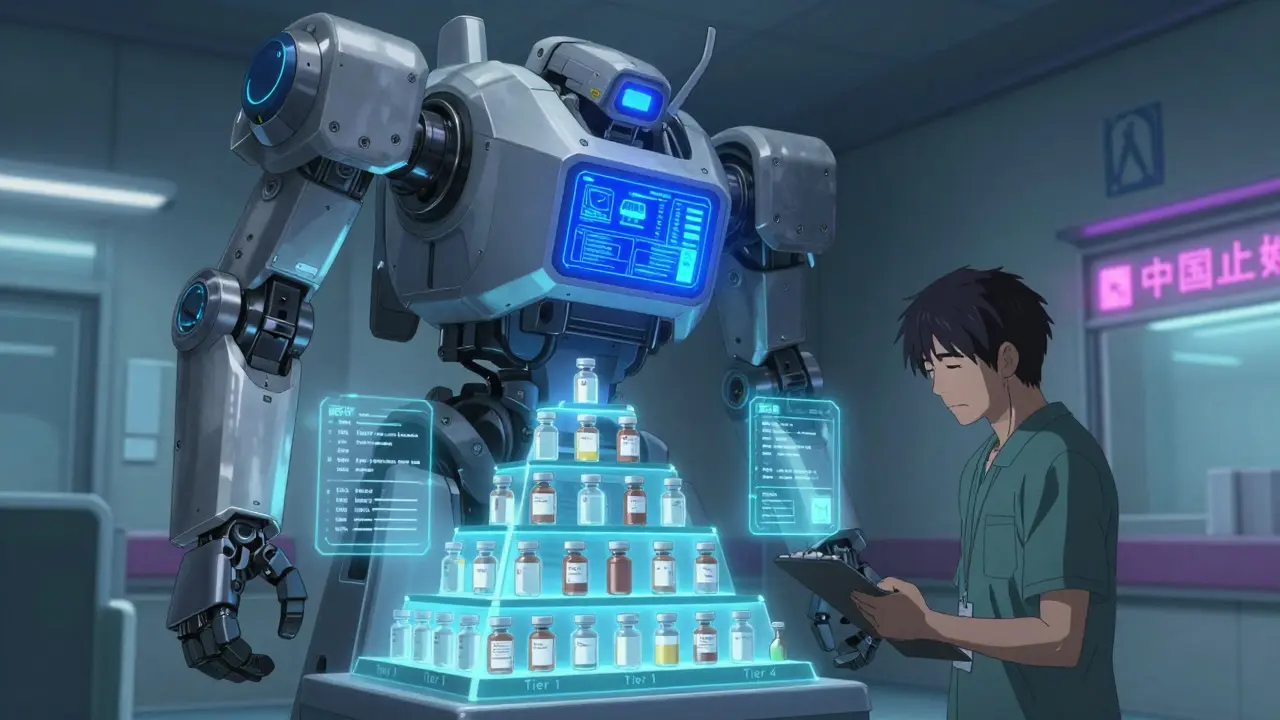
But here’s the catch: states get to pick which drugs are on their list. That list is called a Preferred Drug List (PDL). It’s not just a catalog - it’s a ranking system. Drugs are split into tiers, and your out-of-pocket cost changes depending on where your medicine lands.
How the Tier System Works
Think of your prescription like a hotel. Tier 1 is the economy room. Tier 3 is the suite. Most states use three or four tiers:
- Tier 1: Generic drugs. These are the cheapest. You’ll usually pay $1-$5 per prescription. Most common meds like metformin, lisinopril, or atorvastatin fall here.
- Tier 2: Brand-name drugs with generic alternatives. These cost more - often $15-$30. Your copay jumps because the state wants you to try the cheaper version first.
- Tier 3: Brand-name drugs with no generic. These can cost $40-$100. Think newer diabetes drugs or biologics for rheumatoid arthritis.
- Tier 4 (if used): Specialty drugs. These are the expensive ones - cancer treatments, rare disease therapies, gene therapies. Copays can hit $300+ unless you qualify for extra help.
Some states, like North Carolina, have even more detail. They’ll tell you if a drug is “preferred” or “non-preferred.” If it’s non-preferred, you might need prior authorization just to get it - even if it’s the only one that works for you.
Step Therapy: The “Try Before You Get” Rule
Ever hear of “trial and failure”? That’s step therapy. States require you to try one or two cheaper drugs before they’ll cover the one your doctor prescribed.
Example: Your doctor prescribes Wellbutrin XL for depression. But your state’s formulary says you must first try two other SSRIs - say, sertraline and escitalopram - and they must have failed. Only then will Medicaid approve Wellbutrin. If you tried one and it didn’t work? You still have to try the second. And if you skip this? Your pharmacy won’t fill it.
Thirty-eight states use this rule. North Carolina requires two failed attempts for most drug classes. Florida does too. But some states are more flexible - especially for mental health, epilepsy, or rare diseases.
The goal? Save money. The reality? Many people wait weeks for approval. A 2024 survey by the Medicare Rights Center found 63% of Medicaid users faced delays. The average wait for approval? Over a week. Appeals? Two weeks. That’s not just frustrating - it’s dangerous.

Prior Authorization: What Your Doctor Has to Do
Some drugs aren’t just restricted - they’re locked. To get them, your doctor must submit paperwork. This is called prior authorization.
What’s required? Usually:
- A note from your doctor explaining why the drug is medically necessary
- Proof you tried (and failed) other options
- Lab results or diagnosis codes
For example, if you have Type 1 Diabetes and need premixed insulin, North Carolina allows prior authorization to last up to three years - if your doctor documents ongoing need. But if you switch to a new provider? You might have to start over.
Here’s the kicker: 78% of denied prior authorizations are overturned when the doctor submits full documentation. So if your claim gets denied, don’t give up. Ask your doctor to resubmit with more detail.
Costs You Actually Pay - And How to Lower Them
Most Medicaid enrollees pay little to nothing. But it’s not always zero.
In most states:
- Generics: $0-$5
- Brand-name: $5-$15
- Specialty drugs: $10-$50 (sometimes more)
But if you qualify for Extra Help - a federal program for people with low income - your costs drop even further. In 2026:
- $0 premium
- $0 deductible
- $4.90 copay for generics
- $12.15 for brand-name drugs
- Once you hit $2,000 in total drug costs for the year? You pay $0 for everything else.
Here’s the problem: 1.2 million people eligible for Extra Help don’t even know they qualify. If you have full Medicaid coverage, you automatically qualify. But you have to ask. Call your state Medicaid office. Ask: “Am I eligible for Extra Help?”
Why Your Drug Might Vanish From the List
Formularies change. All the time. In October 2025, North Carolina removed 11 drugs from its preferred list - including Vasotec, Diastat, and Trulance - because they no longer qualified for federal rebates. In July 2025, Epidiolex®, a life-changing epilepsy drug, was moved from preferred to non-preferred. That meant higher costs and more paperwork for hundreds of patients.
Why does this happen? It’s all about money. Drug manufacturers pay rebates to states. If a drug doesn’t offer a big enough rebate, it gets cut. It’s not about safety. It’s about cost.
States also remove drugs that are no longer cost-effective. For example, hepatitis C cures used to cost $80,000 per treatment. Now, with competition and rebates, some cost under $25,000. So older drugs get phased out.

Where to Get Help - And What to Do When Things Go Wrong
You’re not alone. Millions of people struggle with this system. But help exists.
- State Health Insurance Assistance Programs (SHIP): Free counselors who know your state’s rules. Call them. They’ll walk you through prior auth, formularies, and appeals. In 2025, 64% of their calls were about pharmacy issues.
- Your pharmacy: Ask if they’re in-network. If you go to an out-of-network pharmacy, you’ll pay full price - and Medicaid won’t cover it.
- Your doctor: If a drug is denied, ask them to write a letter of medical necessity. Include your diagnosis, failed alternatives, and why this drug is critical.
- Medicaid office: Request a copy of your state’s current formulary. Most post them online. North Carolina’s is updated every July and October.
And if you’re denied? You have the right to appeal. The process usually takes 10-14 days. If you’re sick or in crisis, ask for an expedited review. You don’t have to wait.
What’s Changing in 2026
Things are shifting. In early 2026, CMS will require states to prove their formularies don’t block access to medically necessary drugs. That’s a big deal. It means states can’t just cut drugs because they’re expensive - they have to show there’s a safe, effective alternative.
Also, starting in 2026, Medicaid beneficiaries can change their drug coverage once a month - not just once a year. That gives you more flexibility if a drug is removed or your needs change.
And there’s more: 22 states are now testing new payment models for gene therapies - drugs that cost over $2 million per dose. These programs link payment to outcomes. If the drug works? The state pays. If it doesn’t? They pay less. It’s experimental - but it could change how we pay for life-saving treatments.
Final Takeaways
- Medicaid covers prescriptions - but not all drugs. Each state has its own list.
- You may need to try cheaper drugs first (step therapy).
- Prior authorization is common. Get your doctor involved.
- Generics cost next to nothing. Brands cost more. Specialty drugs cost a lot - unless you qualify for Extra Help.
- Formularies change. Check yours every 6 months.
- If you’re denied, appeal. With proper documentation, most denials get reversed.
- Extra Help is automatic if you have full Medicaid. Ask your state.
Medicaid pharmacy coverage isn’t perfect. But it’s designed to keep people alive - not broke. Knowing how it works is the first step to getting what you need.
Does Medicaid cover all prescription drugs?
No. Medicaid covers outpatient prescription drugs, but each state creates its own list of approved medications called a Preferred Drug List (PDL). While nearly all states cover drugs for all eligible enrollees, some drugs are excluded or require prior authorization. The list changes based on cost, rebates, and clinical guidelines.
Why do I have to try other drugs before getting the one my doctor prescribed?
This is called step therapy or "trial and failure." States require you to try one or two lower-cost, preferred drugs before covering a more expensive brand-name or specialty drug. The goal is to reduce costs while still ensuring access. But exceptions exist - for example, if the only available drug in a class is the one your doctor prescribed, or if you have a documented allergy or failure to other options.
How much will I pay for my prescriptions under Medicaid?
Most Medicaid enrollees pay $0-$5 for generics and $5-$15 for brand-name drugs. Specialty drugs may cost $10-$50 or more. If you qualify for Extra Help (Low-Income Subsidy), your copays drop to $4.90 for generics and $12.15 for brand-name drugs, with $0 cost after you hit $2,000 in annual spending. Some states have $0 copays for all drugs.
Can my Medicaid drug coverage change without notice?
Yes. States update their formularies multiple times a year - often in July and October. If a drug is removed, you’ll usually get a notice from your pharmacy or Medicaid plan. But not always. That’s why it’s important to check your state’s current Preferred Drug List every six months. If a drug you need is removed, you can appeal or ask your doctor to request prior authorization.
Do I have to use a specific pharmacy to get my Medicaid-covered drugs?
Yes. You must use a pharmacy in your state’s Medicaid network. Out-of-network pharmacies won’t bill Medicaid, and you’ll pay full price. Most states have thousands of network pharmacies - including CVS, Walgreens, and local independents. Mail-order pharmacies are often required for maintenance medications like blood pressure or diabetes drugs, as they offer lower costs and automatic refills.
How do I find out what drugs are covered in my state?
Visit your state’s Medicaid website and search for "Preferred Drug List" or "Formulary." For example, North Carolina publishes its PDL online with updates dated July 1 and October 1 each year. You can also call your state’s Medicaid office or ask your pharmacist. Many states offer searchable databases where you can type in your drug name and see its tier and any restrictions.
What if my drug is denied for prior authorization?
You have the right to appeal. Your doctor must submit a letter of medical necessity explaining why the drug is essential - including your diagnosis, past treatment failures, and risks of not using it. With complete documentation, 78% of initial denials are overturned on appeal. If you’re in urgent need, request an expedited review - most states must respond within 72 hours.
Can I get help paying for my medications if I’m on Medicaid?
Yes - if you qualify for Extra Help, a federal program for people with low income. If you have full Medicaid coverage, you automatically qualify. Extra Help lowers your copays to $4.90 for generics and $12.15 for brand-name drugs, with $0 cost after $2,000 in annual spending. Many people don’t know they qualify. Call your state Medicaid office or visit Medicare.gov to confirm your eligibility.
13 Comments
Ashlyn Ellison
My mom’s on Medicaid and just got denied her insulin because it moved to tier 4. We had to appeal. Took three weeks. She nearly skipped doses. This system is broken.
Monica Warnick
Oh please. Like anyone actually reads these formularies. I work in a pharmacy. People come in screaming because their ‘life-saving’ drug got dropped from the list. Meanwhile, the state’s just saving a few bucks on rebates. It’s not about health-it’s about accounting spreadsheets. And don’t even get me started on step therapy. I’ve seen people go blind waiting for approval to switch from one SSRI to another. Like, you’re telling me we’re okay with that?!
And don’t even get me started on the ‘Extra Help’ thing. Half the people who qualify don’t know they’re eligible. Medicaid should auto-enroll them. It’s not a reward program. It’s a lifeline.
North Carolina removed Vasotec? That’s the drug my cousin’s been on for 12 years. Now she’s switching to a ‘preferred’ alternative that gives her migraines. But hey, it’s cheaper. Real compassion.
And why do they even call it ‘preferred’? Like, who’s the judge? Some bean counter who’s never met a patient? This isn’t a Netflix algorithm. People’s lives are on the line.
They say ‘appeals get overturned 78% of the time’-but that’s only after you’ve already waited weeks, missed work, and cried in a pharmacy line. That’s not a system. That’s a torture test.
And the worst part? No one’s talking about how this disproportionately affects rural folks. No pharmacies nearby. No internet access. No one to help them file paperwork. They just… stop getting meds. And then they show up at the ER with a heart attack. And guess who pays?
It’s not about cost-effectiveness. It’s about who gets to suffer quietly.
Scott Conner
wait so if u have medicaid u automatically get extra help? that sounds too good to be true. i thought u had to apply or something. also is this like the same as ssi or different? lol
Ken Cooper
Yup, if you’re on full Medicaid, you’re automatically eligible for Extra Help-no extra form, no background check. It’s one of those things the government *says* it wants to help you with… but then makes it so confusing you give up. I’ve helped three friends get this, and all of them were shocked. One lady said she’d been paying $90/month for her asthma inhaler… until I told her to call Medicaid. Now she pays $4.90. She cried. I cried. We all cried.
And yes, it’s separate from SSI, but if you get SSI, you usually get Medicaid too. So it’s like a double win. The system’s weird, but this one part? Actually works. Just… no one tells you.
Pro tip: Call your state’s Medicaid office and ask, ‘Am I eligible for the Low-Income Subsidy for prescriptions?’ Don’t say ‘Extra Help.’ They might not know the term. Say ‘Low-Income Subsidy.’ It’s the official name. Works every time.
Also-check your formulary every six months. I had a guy come in last month because his blood pressure med got downgraded. He didn’t know until his pharmacy refused to fill it. He thought the pharmacy was ‘hating on him.’ Nope. Just the state’s spreadsheet updated.
And if you’re on a specialty drug? Ask your doctor to write a letter with your diagnosis, your history of failed alternatives, and a note that says ‘This is medically necessary.’ That’s the magic combo. 78% of denials get overturned. Don’t quit. Fight.
Frank Baumann
THIS IS WHY PEOPLE DIE. I’VE SEEN IT. I WORK IN A HOSPITAL. I’VE SEEN PEOPLE COME IN WITH KIDNEY FAILURE BECAUSE THEY WEREN’T ABLE TO GET THEIR DIABETES MEDS. THEY WERE TOLD TO TRY TWO OTHER DRUGS FIRST. THEY DID. THEY FAILED. THEN THEY HAD TO WAIT TWO WEEKS FOR APPROVAL. TWO WEEKS. WHILE THEIR BLOOD SUGAR SPUN OUT OF CONTROL. WHILE THEIR NERVES DIED. WHILE THEIR FEET WENT NUMB.
AND THEN THEY’RE SURPRISED WHEN THEY END UP ON DIALYSIS?
THIS ISN’T A ‘SYSTEM.’ IT’S A HUMAN RIGHTS ABUSE.
THEY SAY ‘IT’S ABOUT COST.’ NO. IT’S ABOUT POLITICS. IT’S ABOUT WHO GETS TO BE SICK IN SILENCE. IT’S ABOUT WHO GETS TO BE IGNORED.
I’VE SEEN A 72-YEAR-OLD WOMAN CRY BECAUSE SHE COULDN’T GET HER RHEUMATOID ARTHRITIS DRUG. SHE COULDN’T WALK. SHE COULDN’T HOLD HER GRANDCHILDREN. SHE HAD TO WAIT 17 DAYS FOR PRIOR AUTHORIZATION. AND WHEN SHE FINALLY GOT IT? HER DOCTOR HAD TO REWRITE THE FORM BECAUSE THE FIRST ONE HAD A TYPO.
TYPO.
WE’RE DOING THIS TO OUR PEOPLE.
AND THE WORST PART? NO ONE’S LISTENING.
Susan Kwan
Wow. So Medicaid covers drugs… but only if you jump through enough hoops to qualify for a PhD in bureaucracy. Congrats, America. You’ve turned healthcare into an obstacle course designed by someone who hates poor people.
And the ‘Extra Help’ thing? Yeah, right. Like anyone with a 9-to-5 and two kids is gonna have time to call Medicaid, fill out forms, and argue with a voicemail system that says ‘press 5 for Spanish’-but 5 doesn’t exist.
Also, ‘formularies change every 6 months’? So what? You’re telling me a woman on insulin gets a letter saying, ‘Your drug is now non-preferred’… but she’s got no idea what that means? And the pharmacy just says ‘sorry, we can’t fill it’? No explanation? No help?
And don’t even get me started on rural areas. My cousin lives in West Virginia. Her nearest pharmacy is 45 miles away. She can’t drive. No bus. No internet. No phone service. How’s she supposed to appeal? Write a letter? In crayon?
This isn’t healthcare. It’s performance art. And we’re all just watching.
Tom Forwood
As someone who’s worked in public health for 15 years, I’ve seen this play out in every state. The real tragedy isn’t the tier system-it’s that we treat medication like a luxury. It’s not. It’s survival. Metformin isn’t a ‘nice-to-have.’ It’s a ‘live or die.’
And the step therapy? It’s not just inefficient-it’s cruel. Imagine being told you have to try three different antidepressants before they’ll let you take the one that actually works. And if one fails? You start over. Like you’re playing a video game where the boss resets every time you lose.
Meanwhile, drug companies are paying rebates to states… and states are using that money to cut other services. So the cycle continues: we cut mental health services, so more people need meds. We cut meds, so more people end up in ERs. We pay more. Everyone loses.
And the worst part? The people who scream the loudest about ‘waste’ are the ones who’ve never had to choose between insulin and rent.
We need to stop treating medication like a privilege. It’s a human right. And if you’re on Medicaid? You’re not asking for charity. You’re asking for dignity.
Tricia O'Sullivan
Thank you for this comprehensive overview. The clarity with which you have presented the structural challenges within Medicaid's pharmaceutical coverage is both enlightening and deeply concerning. It is imperative that public policy evolves to reflect the human cost of administrative barriers, particularly for vulnerable populations who rely on these services for essential care.
While the tiered formulary system may offer fiscal efficiency, its implementation often lacks the necessary safeguards to ensure equitable access. The requirement for prior authorization and step therapy, though intended to reduce expenditure, inadvertently introduces delays that may precipitate acute health crises.
It is also noteworthy that the automatic eligibility for Extra Help under full Medicaid coverage remains underutilized, likely due to insufficient outreach and communication. A centralized, proactive notification system-perhaps integrated with existing Medicaid renewal processes-could significantly improve uptake.
Ultimately, healthcare is not a commodity. Access to life-sustaining medication must be treated as a fundamental right, not a bureaucratic hurdle.
MANI V
Ugh. Another entitled American whining because they can’t get their $1000/month drug for free. In India, we have generic drugs for pennies. People live with diabetes, hypertension, even cancer… and they don’t have Medicaid. They just take the medicine. No forms. No appeals. No drama.
Why can’t you just take the generic? Why do you need the ‘brand name’? Is it because you’re addicted to fancy packaging? Or just because you think you’re special?
My sister in Delhi takes a $2/month drug for her blood pressure. She’s 68. Still walks 5km daily. You’re in the US with Medicaid and you’re crying because you have to wait 10 days for a drug that costs $50? Grow up.
Stop being so entitled. The system isn’t broken. You are.
Ritteka Goyal
Bro in India we have 1000x better access to meds than you guys. We don’t need 5 forms and 3 doctors to get our diabetes pills. My aunt takes a $1.50 pill every day. She’s 72. No insurance. No paperwork. Just walks to the local chemist. You Americans are so soft. You cry because you have to wait 2 weeks for your insulin? We wait 2 years for hospitals. We don’t complain. We just take what we can get.
And why do you need brand name drugs? You think your body is special? Your liver doesn’t care if it’s branded or generic. It just wants to work. Stop being dramatic.
Also, Extra Help? That’s just another American entitlement. In India, if you can’t afford medicine, you don’t get it. You die. Simple. No bureaucracy. No appeals. No drama. Just life.
Maybe if you stopped being so lazy and started walking to the pharmacy instead of waiting for the system to hand you everything, you’d be better off.
Also, why are you even on Medicaid? You should be working. Stop being a burden. India doesn’t have this problem because we don’t coddle people. We build resilience. You need to grow up.
Jonah Mann
sooo… if i have medicaid and im on insulin, i pay $4.90? and after $2000 i pay 0? wait wait wait… that sounds too good. is this real? or is there a catch? like… do i have to sign up for extra help? or is it automatic? because my cousin got denied and she’s on medicaid…
also, is this for all states? what if i live in alaska? or texas? does it change? because i heard some states are worse…
and what about mail order? do i have to use that? my pharmacy said i had to… but i dont wanna wait 2 weeks for my meds…
and why do they change the list in july and october? like… why not january? why not every 3 months? this is so confusing.
Lyle Whyatt
As someone who’s lived in three different states and had to navigate this mess in each one, let me just say: this system is a Rube Goldberg machine designed by someone who hates people.
It’s not about the drugs. It’s about the paperwork. I once spent 11 hours on the phone with my state’s Medicaid office trying to get approval for a drug that was on the formulary… but the form they needed had a typo in the code. The person on the line said, ‘We’ll send you a new form.’ I waited 14 days. Then I called again. They said, ‘Oh, we sent it.’ I never got it.
My doctor had to fax it. Twice. Then I had to hand-deliver a copy to the pharmacy. The pharmacist said, ‘We’ve never seen this form before.’
And then? I got the drug. Two weeks late. My blood sugar was sky-high the whole time.
And now? The drug got moved to tier 3. My copay went from $10 to $45. I’m supposed to switch? But the alternative gives me nausea. So I appeal. Again.
It’s not a healthcare system. It’s a full-time job.
And the worst part? No one’s talking about how this eats away at mental health. I’m not just managing diabetes. I’m managing anxiety. I’m managing rage. I’m managing grief.
And I’m tired.
Ken Cooper
Replying to @7568: Yes, it’s real. No catch. If you have full Medicaid, Extra Help is automatic. No application. Just call your state’s Medicaid office and say, ‘I’m on Medicaid-am I eligible for the Low-Income Subsidy for prescriptions?’ They’ll confirm it. If they say no? Demand to speak to a supervisor. It’s a federal rule. They’re legally required to tell you.
And yes, it’s the same in all states. The copays are federally capped: $4.90 generics, $12.15 brand-name. But some states add *extra* help on top-like $0 copays for everyone. Check your state’s website. Mine (Oregon) does.
Mail-order? Not mandatory. But if you’re on maintenance meds (blood pressure, diabetes, etc.), it’s smarter. You get 90-day supplies. Cheaper. Fewer trips. And they auto-refill. I switched and saved 40%.
And the July/October changes? That’s when drug rebate contracts renew. States update formularies to match new deals. It’s not random. It’s corporate math. But they’re not required to notify you. That’s the flaw.
So check your formulary every six months. Bookmark it. Print it. Share it. Because no one else will.