Every year, more than 1.5 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these errors are preventable - not because doctors or pharmacists made a slip-up, but because patients didn’t know what to ask or what to look for. You don’t need a medical degree to protect yourself. You just need to know a few key terms and how to use them. These aren’t fancy jargon. They’re simple words that give you real power over your own health.
Know the Eight Rights of Medication Safety
The foundation of medication safety isn’t a single rule - it’s a checklist. Originally, nurses used the "Five Rights" to make sure patients got the right medicine: right patient, right drug, right dose, right route, right time. But over time, experts realized that wasn’t enough. Today, the full list includes eight rights. If you can remember and ask about these, you cut your risk of a harmful error in half.
- Right patient: Make sure they check your name and date of birth - not just your first name. Hospitals and clinics are required to use two identifiers. If they only ask "Are you John?" - say no. Ask them to confirm your full name and birth date.
- Right medication: Ask for both the brand name and the generic name. For example, if you’re given "Lipitor," ask if it’s atorvastatin. Similar-sounding names like "Hydroxyzine" and "Hydralazine" cause 23% of medication errors.
- Right dose: Don’t assume the pill looks right. Ask: "How many milligrams is this?" For liquids, especially for kids, ask how to measure it correctly. A teaspoon isn’t always 5ml - some spoons hold more.
- Right route: Is this meant to be swallowed, injected, applied to the skin, or inhaled? A 2019 study found that 12% of serious errors happened because a drug meant for IV use was given by mouth. If it’s a shot, ask: "Where will this go?"
- Right time: Are you supposed to take this with food? At bedtime? Every 8 hours? Write it down or set a phone alarm. People who track their doses improve adherence by 42%.
- Right reason: This is the most important one. Ask: "Why am I taking this?" If your doctor says "for high blood pressure," ask: "What number should it bring down?" Patients who understand why they’re on a drug are 37% less likely to get the wrong one.
- Right documentation: Ask if your medication list was updated in your chart. If you’re being discharged from the hospital, request a written list of everything you’re supposed to take - and compare it to what you’re actually carrying home.
- Right response: Pay attention to how you feel. Are you sleeping better? Is the pain less? Or are you dizzy, nauseous, or breaking out in a rash? Track changes. Patients who monitor their responses reduce severe reactions by 35%.
Understand What an Adverse Drug Event Is
An "adverse drug event" (ADE) sounds technical, but it’s simple: it’s when a medicine hurts you. Not every side effect is an ADE. Feeling a little dry mouth from a blood pressure pill? That’s a side effect. But if that same pill causes your kidneys to fail? That’s an ADE. The CDC says ADEs are one of the biggest preventable health problems in the country. They’re not rare. They happen because of mistakes - wrong dose, wrong drug, or not knowing you’re allergic.
Here’s what to do: When you get a new prescription, ask: "What are the warning signs I should watch for?" Write them down. If you feel something unusual - chest tightness, swelling, sudden confusion - don’t wait. Call your doctor or pharmacist. Don’t assume it’s "just a side effect." If you’re unsure, it’s better to check.
Know Which Medications Are High-Risk
Not all medicines are equal. Some are called "high-alert medications" because even a small mistake can kill. These include:
- Insulin
- Blood thinners like warfarin or apixaban
- Opioids like oxycodone or fentanyl
- IV chemotherapy drugs
- Concentrated electrolytes like potassium chloride
According to ISMP, these drugs cause 67% of fatal medication errors. That doesn’t mean you shouldn’t take them - it means you need to be extra careful. Always ask: "Is this a high-alert drug?" Then double-check the name, dose, and reason. If you’re giving one to a loved one, make sure someone else confirms the details too. Two sets of eyes are better than one.
Recognize a Close Call - and Speak Up
A "close call" is when something almost went wrong - but didn’t. Maybe the nurse almost gave you the wrong pill, but caught it at the last second. Maybe your pharmacy sent you the wrong strength, but you noticed the label didn’t match your old bottle.
Don’t brush these off. They’re not "luck." They’re warnings. If you spot a close call, tell someone. Say: "I think there was a mistake here. Can we check this again?" Hospitals and clinics track these reports to fix systems. Your voice helps prevent the next mistake - maybe even for someone else.
What About Sentinels? Why Should You Care?
The Joint Commission calls a "sentinel event" a serious, unexpected incident - like death or permanent harm - caused by a medical error. A medication error that kills someone? That’s a sentinel event. It sounds scary, but it’s not just for hospitals to worry about. It’s a reminder that these errors happen, and they’re preventable.
If you’ve had a loved one die after a hospital stay and you suspect medication was involved, you’re not alone. Thousands of families face this. Knowing these terms gives you the language to ask: "Was this a preventable error?" You’re not accusing anyone. You’re seeking truth - and pushing for change.

How to Use These Terms in Real Life
Knowing the words isn’t enough. You have to use them - in real conversations. Here’s how:
- Before you leave the doctor’s office, say: "Can you please go over the Eight Rights for this new medicine?"
- At the pharmacy, ask: "Is this the right drug? What’s the generic name? What’s it for?"
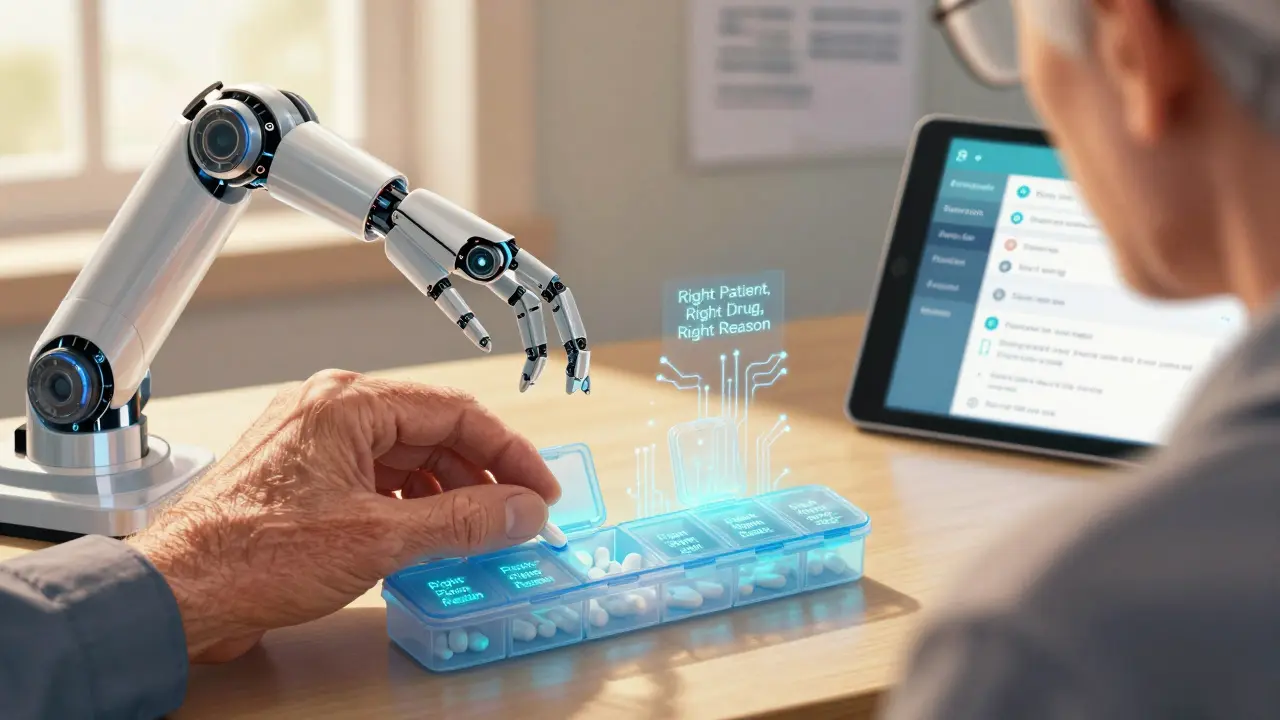
- When you get home, put the meds in a pill organizer with the reason written on each slot.
- Use a free app like Medisafe - it reminds you when to take pills and checks them against the Eight Rights before each alert.
- Bring your full list of meds - including vitamins and supplements - to every appointment. Don’t rely on memory.
Studies show that patients who do this reduce their risk of an ADE by up to 50%. That’s not a small number. That’s life-changing.
Barriers Are Real - But You Can Overcome Them
Not everyone can read medical labels. The National Assessment of Adult Literacy found only 12% of U.S. adults have strong health literacy. That means most people struggle to understand instructions like "take 1 tablet by mouth twice daily."
That doesn’t mean you’re alone. Ask for help. Say: "I’m not sure I understand. Can you explain this in simpler terms?" Many clinics now offer multilingual safety materials. Ask for a translator if you need one. You have the right to understand your care.
What’s Changing in 2025?
Medication safety is getting better - slowly. In 2024, the Joint Commission made it mandatory for hospitals to teach patients the Eight Rights before discharge. The FDA now includes plain-language guides in every new drug package. And apps like Medisafe, used by over 8 million people, now have built-in checks based on these terms.
By 2030, the CDC wants 90% of patients to know at least five of these terms. Right now, only 43% do. You can be part of the change. Start today.
What’s the difference between a side effect and an adverse drug event?
A side effect is a known, often mild reaction to a medicine - like dry mouth, drowsiness, or nausea. An adverse drug event (ADE) is when a medicine causes serious harm - like an allergic reaction, organ damage, or a dangerous interaction. Not all side effects are ADEs, but all ADEs start with a reaction. If you feel something new, strong, or scary, don’t ignore it.
Do I need to know all eight rights to be safe?
You don’t need to memorize them all at once. Start with the top three: right patient, right drug, right reason. Once you’re comfortable, add right dose and right time. The rest follow naturally. The goal isn’t perfection - it’s awareness. Even asking one question - "Why am I taking this?" - can save your life.
What if my doctor gets annoyed when I ask questions?
A good doctor expects questions. If someone gets upset when you ask about your meds, that’s a red flag. You’re not being difficult - you’re being smart. You have the right to understand your treatment. If you feel dismissed, find a new provider. Your health isn’t negotiable.
Can I use these terms for my elderly parents or children?
Absolutely. In fact, you should. Children and older adults are at higher risk for medication errors. For kids, always ask: "What’s the dose based on? Weight or age?" For older adults, check for interactions - many take five or more drugs. Use the Eight Rights as your checklist when helping them take pills. You’re not replacing their care - you’re protecting it.
Are there free tools to help me track my meds?
Yes. Apps like Medisafe, MyTherapy, and even Apple Health let you log your medications, set reminders, and share lists with family or doctors. Many include built-in checks for the Eight Rights. You can also print a free medication list from the CDC website and keep it in your wallet. Paper works too.
What should I do if I think I got the wrong medicine?
Don’t take it. Call your pharmacy first. If they say it’s correct but you’re still unsure, call your doctor. Take the bottle with you to the appointment. Never guess. Even if you’ve taken it before, doses and brands change. Your safety isn’t worth the risk.
8 Comments
Olivia Goolsby
Okay, so let me get this straight: the government, hospitals, and Big Pharma want us to believe that if we just memorize eight stupid rights, we’ll magically be safe from poisoning ourselves?!! I’ve seen the forms-they’re written in 6-point font, with tiny checkboxes, and the pharmacist won’t even look you in the eye. And don’t get me started on the ‘free apps’-they’re all data-harvesting tools disguised as safety aids. They track your pills, your sleep, your heart rate, then sell it to insurers who jack up your premiums because you ‘took too many opioids.’ This isn’t safety-it’s surveillance wrapped in a pink ribbon. They want you to think you’re empowered… while they quietly remove the right to sue when you’re left in a coma because someone misread ‘Lipitor’ as ‘Lithium.’
Alex Lopez
While I appreciate the enthusiasm behind this piece, I must respectfully note that the Eight Rights framework, though well-intentioned, is often impractical in high-volume clinical settings where nurses manage 12+ patients per shift. That said, your emphasis on patient engagement is commendable. I’d suggest pairing this checklist with a standardized verbal confirmation protocol-e.g., ‘Tell me in your own words what this pill is for.’ That’s been shown in JAMA studies to reduce errors by 41%. Also, emoticons are not a substitute for clarity, but 😊 here for encouragement. Keep asking questions. You’re not a burden-you’re a vital part of the care team.
Gerald Tardif
This is the kind of info that should be handed out like gum at a pharmacy. Not everyone’s got a medical degree, but everyone’s got a brain-and a right to not get poisoned by a typo. I’ve seen grandmas take insulin because they thought it was for ‘sugar problems’ and didn’t know it was for blood sugar. I’ve seen kids given adult doses because the bottle said ‘for children 6+’ but didn’t say ‘per 10 lbs.’ This isn’t rocket science. It’s basic human decency. If you’re reading this and you’re scared to ask, just say: ‘I’m not a doctor, but I’m trying to stay alive.’ That’s enough. You’re already doing better than most.
Monika Naumann
It is truly regrettable that Western societies have allowed their citizens to become so dependent on external systems for basic health literacy. In India, we have long understood that health is a personal responsibility. We do not wait for apps or government pamphlets to tell us how to take medicine. We learn from our elders, from tradition, from experience. That this article even needs to exist speaks volumes about the erosion of cultural wisdom in your country. Why are you not taught these things in school? Why are you not encouraged to memorize the names of your medicines as you memorize your own phone number? This is not a system failure-it is a moral failure.
Elizabeth Ganak
Love this! I’ve been using Medisafe for my mom since she started on five meds after her stroke. She used to mix up her blood pressure pills and her thyroid ones-now she gets a little chime and a picture of the pill. She even started reminding me when I forget my vitamins. 😊 The Eight Rights? I just say them out loud when I hand her the bottle: ‘Right person? Yep, Mom. Right drug? Atorvastatin. Right reason? To keep your heart happy.’ It sounds silly, but it works. And no one’s ever gotten mad at me for asking. Honestly? They’re usually relieved someone finally cares enough to check.
Nicola George
So… we’re supposed to be the human error-checking system for a broken healthcare machine? Cool. I’ll just add ‘medication interrogator’ to my resume. 😏 Look, I get it-asking questions saves lives. But let’s be real: if your doctor gets annoyed when you ask what your pill is for, maybe your doctor’s the problem. And if your pharmacist can’t tell you if that blue pill is 10mg or 20mg without checking the computer three times? Maybe your pharmacy’s the problem. You’re not the glitch-you’re the patch. Keep asking. And if they roll their eyes? Smile. Then go to the next clinic. There’s always one that doesn’t treat you like a liability.
Raushan Richardson
YES. This. I used to think I was being ‘difficult’ for asking about my meds. Then my cousin had a bad reaction because no one told her the new painkiller interacted with her antidepressant. She ended up in ICU. That’s when I started using the Eight Rights like a mantra. Now I do it for my whole family. I print out the list, stick it on the fridge, and we go through it every Sunday. My 78-year-old dad even started correcting the nurses. 😎 It’s not complicated. It’s just… not taught. So we teach each other. And if you’re reading this and you’re scared? Start with one question. Just one. ‘Why am I taking this?’ That’s your superpower. Use it.
Robyn Hays
One tiny thing the article didn’t mention: what if you’re nonverbal? Or have dementia? Or your child is too young to speak? The Eight Rights are great-but they assume you can speak up. I’ve seen families struggle when Grandma can’t remember her meds, or when the autism diagnosis means your kid won’t swallow pills without a meltdown. What’s the protocol then? Maybe we need a ‘Right Advocate’-someone trained to speak for those who can’t. Hospitals should have volunteer advocates on call for these cases. And yes, I’m volunteering. If you’re reading this and you’ve ever sat in a hospital waiting room wondering if your loved one was getting the right pill… you’re not alone. Let’s make this system work for everyone-not just the loud ones.