When you’re on a medication that keeps you alive-like a transplant patient on immunosuppressants or someone with epilepsy taking anticonvulsants-the difference between a pill working and a pill harming you can be as small as a fraction of a milligram. These are narrow therapeutic index drugs, or NTI drugs. They’re not just any pills. They’re the ones where even tiny changes in how your body absorbs the drug can lead to serious harm: organ rejection, seizures, dangerous bleeding, or heart rhythm problems. And when it comes to switching from a brand-name version to a generic, the stakes are higher than almost any other type of medication.
What Makes a Drug Have a Narrow Therapeutic Index?
A narrow therapeutic index means the gap between the dose that works and the dose that’s toxic is extremely small. The FDA defines NTI drugs as those where small changes in blood concentration can cause serious, even life-threatening, side effects or treatment failure. For example, if your blood level of tacrolimus drops just 10%, your body might reject your new kidney. If it rises 10%, you could develop kidney damage or nerve problems.
These drugs don’t have a wide safety buffer. Unlike antibiotics or blood pressure pills, where you can take a little more or less without big consequences, NTI drugs require precision. That’s why doctors and pharmacists don’t just pick any generic-they look at the specific manufacturer, the formulation, and sometimes even the batch number.
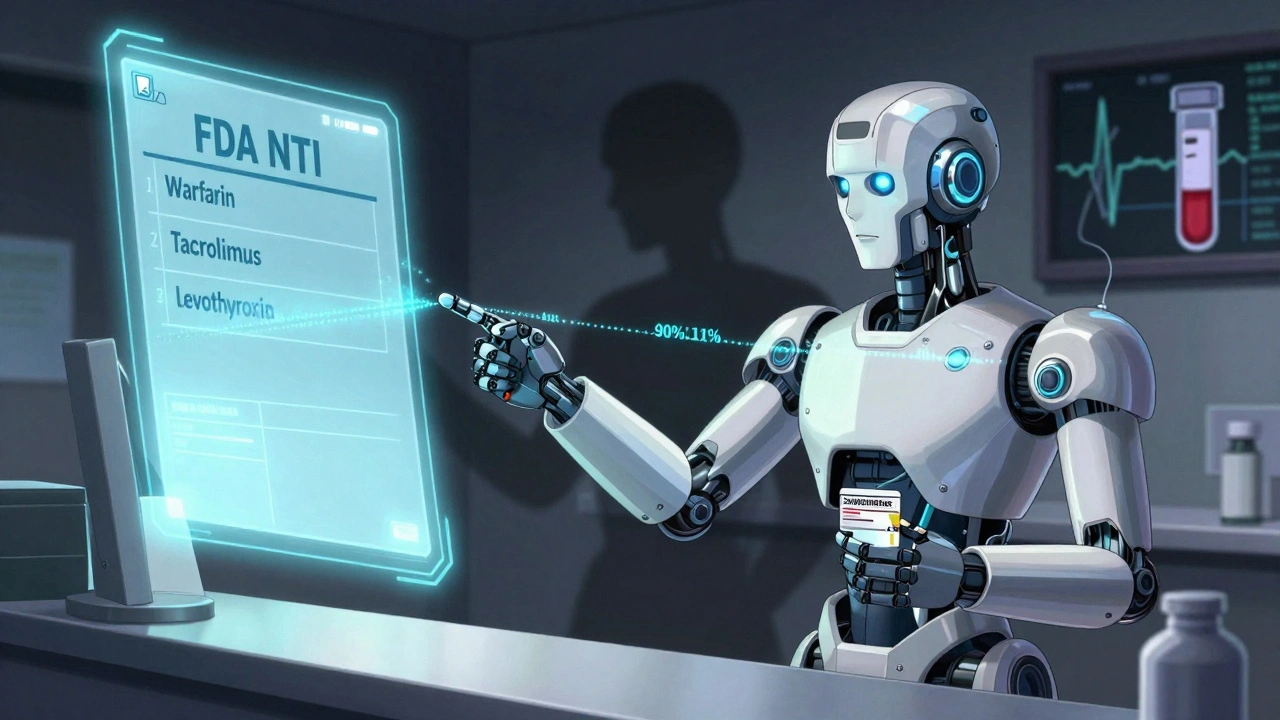
Common NTI drugs include:
- Warfarin (blood thinner)
- Tacrolimus and cyclosporine (transplant immunosuppressants)
- Phenytoin and carbamazepine (anti-seizure meds)
- Digoxin (heart rhythm control)
- Levothyroxine (thyroid hormone)
- Aminoglycosides (antibiotics like gentamicin)
- Targeted cancer drugs like nilotinib and axitinib
The FDA officially lists 33 drug products (14 active ingredients) as NTI as of early 2024. That number keeps growing as newer cancer drugs and biologics are added to the list.
Why Generic Substitution for NTI Drugs Is Risky
For most medications, generics are just as safe and effective as brand names. The FDA requires them to be bioequivalent-meaning they deliver the same amount of drug into your bloodstream within an acceptable range: 80% to 125% of the brand. That’s a wide window. For NTI drugs, that window is too wide.
For NTI drugs, the FDA demands much tighter standards. If the brand drug has low variability in how patients absorb it, the generic must match within 90% to 111%. In some cases, like with levothyroxine, the requirement is even stricter: 95% to 105%. That’s because even a 10% drop in absorption could mean your thyroid levels go out of control.
Here’s the catch: two different generic versions of the same NTI drug can have different absorption rates. One might be 97% bioavailable, another 103%. That’s within FDA rules for NTI drugs-but for you, it could mean a trip to the ER. Many patients report wild swings in blood levels after switching between generics or from brand to generic. A transplant patient on Reddit shared that switching from Prograf to generic tacrolimus caused their creatinine to double in three weeks. Another person on PatientsLikeMe said they’ve been stable on generic phenytoin for five years. Both are real. But the difference? Consistency.
How Pharmacists and Doctors Handle NTI Drugs
Most pharmacists are cautious. A national survey found only 28% of pharmacists are comfortable substituting a generic for an NTI drug on the first prescription, compared to 78% for regular drugs. Why? Because they’ve seen the consequences. One hospital pharmacist on Reddit said they’ve had patients on levothyroxine go from a TSH of 2.5 to 12.0 after a generic switch-meaning their thyroid went from normal to severely underactive.
Doctors often write “dispense as written” on prescriptions for NTI drugs. That means the pharmacy can’t swap the brand for a generic without calling them back. Some states have laws backing this up: as of 2023, 42 U.S. states restrict automatic substitution of NTI drugs. But the rules vary. In some places, pharmacists can substitute if the prescriber doesn’t object. In others, they can’t substitute at all.
Therapeutic drug monitoring (TDM) is standard for NTI drugs. That means regular blood tests to check levels. If you’re on tacrolimus, your doctor will likely check your blood level every few weeks when you start, then every 1-3 months after you’re stable. If you switch products-even to another generic-you’ll need another test.
The Cost vs. Safety Trade-Off
Generic drugs save money. A lot of it. Brand-name tacrolimus can cost $1,200 a month. The generic? Around $150. For many patients, that’s the difference between taking the drug or skipping doses. But for NTI drugs, the savings can come with hidden costs.
Switching products might mean extra doctor visits, more blood tests, hospital stays, or emergency care. One study found patients with heart failure or diabetes had a 30% higher risk of drug-related problems when taking NTI generics. The financial burden isn’t just the price of the pill-it’s the cost of managing the fallout if something goes wrong.
That’s why some patients and providers prefer to stick with one product-brand or generic-and never switch. The FDA recommends this too. Once you’re stable on a specific version, staying on it is safer than swapping for a cheaper one.
What You Should Do If You’re on an NTI Drug
If you’re taking a narrow therapeutic index drug, here’s what you need to know:
- Know your drug. Is it on the FDA’s NTI list? Check the FDA’s website or ask your pharmacist. Don’t assume all generics are equal.
- Ask about substitution. Before you fill a prescription, ask: “Is this the same brand/generic I’ve been taking?” If it’s different, ask why. You have the right to refuse a switch.
- Get blood tests. If you switch products-even to another generic-ask your doctor to check your blood levels within 2-4 weeks. Don’t wait for symptoms.
- Keep a record. Write down the name of the drug, the manufacturer, and the lot number if you can find it. If you have a bad reaction, that info matters.
- Don’t assume “generic” means “same.” For NTI drugs, that’s not true. Two generics of the same drug can behave differently in your body.
Some patients do fine on generics. But the key is consistency. If you start on a generic and stay on it, you’re likely okay. The risk comes from switching back and forth between brands and generics-or between different generic manufacturers.
The Future of NTI Drugs and Generics
The FDA is working on more detailed guidelines for newer NTI drugs, especially cancer treatments. By 2025, they plan to release 12 new product-specific guidances. That means stricter, more tailored rules for each drug, not just a one-size-fits-all approach.
Pharmacogenomics is also changing the game. Some patients metabolize drugs faster or slower based on their genes. By 2028, experts predict 40% of NTI drug prescriptions will include genetic testing to tailor the dose. That could make generics safer by personalizing the dose instead of forcing everyone into the same narrow window.
But international differences remain. The FDA, European Medicines Agency, and Japan’s drug agency all have different ways of defining NTI drugs. That makes global drug development harder and can lead to different generic versions being sold in different countries.
For now, the safest path is simple: know your drug, stay on the same version, and never assume a generic is interchangeable without checking. Your life might depend on it.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe. Many patients take generic NTI drugs safely for years. The issue isn’t generics themselves-it’s switching between different versions. If you start on a generic and stay on that same generic (same manufacturer, same formulation), your body adapts. The risk comes from switching between brand and generic, or between two different generics. Consistency matters more than the name on the bottle.
Can my pharmacist switch my NTI drug without telling me?
It depends on your state. In 42 U.S. states, pharmacists are legally restricted from automatically substituting NTI drugs without the prescriber’s permission. But in the other eight, they can substitute unless the doctor writes “dispense as written.” Always ask your pharmacist if your prescription was switched. You have the right to know.
Why do some people do fine on generics while others have problems?
It comes down to individual biology and consistency. Some people absorb drugs very predictably. Others have gut issues, take other medications, or have genetic differences that affect how their body handles the drug. If you’ve been stable on one version for months or years, your body is used to it. Switching-even to a different generic-can throw off that balance. It’s not about the drug being bad; it’s about your body’s sensitivity to small changes.
How often should I get blood tests if I’m on an NTI drug?
When you start an NTI drug, your doctor will likely check your blood levels every 1-2 weeks until you’re stable. After that, every 1-3 months is typical. If you switch products-even to another generic-you should have a blood test within 2-4 weeks. Don’t wait for symptoms like fatigue, dizziness, or irregular heartbeat. By then, it might be too late.
What should I do if I think my generic NTI drug isn’t working?
Don’t stop taking it. Call your doctor or pharmacist right away. Tell them you’ve noticed new symptoms or feel different. Ask if your medication was recently switched. Request a blood test to check your drug levels. Keep a log of when you started the new version and when symptoms began. This helps your provider decide whether to switch you back or adjust your dose.
Final Thoughts
Narrow therapeutic index drugs aren’t just another prescription. They’re precision tools. One wrong move, and the outcome can be catastrophic. Generics play a vital role in making healthcare affordable-but for NTI drugs, affordability shouldn’t come at the cost of safety. The best approach is simple: know what you’re taking, stick with the same version, and never let a switch happen without your knowledge. Your health isn’t a cost-saving experiment. It’s your life.
12 Comments
Akash Sharma
I’ve been on tacrolimus since my liver transplant in 2018, and I switched from Prograf to a generic after my insurance changed. At first I felt fine-no symptoms, no issues. But after three months, my kidney function started creeping up. My nephrologist ordered a blood test and found my levels had dropped 15%. Turns out the new generic was from a different manufacturer, and even though it was FDA-approved, my body just didn’t absorb it the same way. Now I’m back on the brand, and I don’t care how much it costs. My life isn’t a budget spreadsheet. I wish more people understood that generics aren’t just ‘cheaper versions’-they’re different chemical experiences for some of us.
Also, I keep a little notebook with the lot number, manufacturer, and date I started each bottle. It’s saved me twice now when things went sideways. If you’re on an NTI drug, do this. It’s not paranoia-it’s survival.
Mark Gallagher
Stop the hysteria. The FDA regulates generics with the same rigor as brand-name drugs. If you’re having issues, it’s not the generic-it’s your noncompliance, your poor diet, or your failure to follow up with blood work. I’ve worked in pharmacy for 22 years and I’ve never seen a single case where a properly manufactured generic caused harm. The real problem is patients who panic every time the pill color changes. You’re not special. Your body isn’t fragile. Stop blaming the system and take responsibility.
Wendy Chiridza
My mom’s on levothyroxine and switched generics last year. Her TSH went from 2.1 to 8.9 in six weeks. No symptoms at first-just fatigue. Then depression. Then weight gain. She didn’t realize it was the pill until she checked the label. We called the pharmacy-they said it was ‘therapeutically equivalent.’ Equivalent doesn’t mean identical. The FDA’s 95-105% window is a joke when your thyroid is your entire metabolism. Doctors need to stop assuming patients will catch the change. We need mandatory notification when a switch happens. Period.
Gerald Nauschnegg
Look I get it. I’ve been on carbamazepine for 12 years. I’ve been on three different generics. One made me feel like I was walking through molasses. Another gave me vertigo for two weeks. The third? Perfect. I didn’t know why until I started reading the manufacturer info. Turns out one was made in India, one in Canada, one in the US. The Canadian one was the worst. The US one? Best. So now I only take the one with the same logo on the bottle. I don’t care if it costs $50 more. I’d rather pay extra than end up in the ER again. If you’re on an NTI drug, don’t just trust the pharmacist. Look at the name on the pill. Write it down. Make it your ritual.
Joanne Rencher
Ugh. Another one of these posts. Like we didn’t already know generics can be sketchy. Can we move on? I’m tired of being lectured about my thyroid pills. Just give me the cheapest one and shut up. If I die, I die. At least I saved $1000 this month.
Adrianna Alfano
As someone who’s been on warfarin since I was 28 and had a pulmonary embolism-I’m so glad someone finally wrote this. I used to get angry when my pharmacist would swap my Coumadin for a generic. But then I learned: it’s not about trust, it’s about control. I keep a log. I get INR tested every week when I switch. I call my doctor before I take the first pill of a new batch. I don’t care if I sound obsessive. I’m alive because I’m obsessive. To anyone on an NTI drug: you’re not crazy. You’re smart. And if someone tells you it’s ‘just a pill,’ they’ve never had to live with the consequences of one wrong dose.
Also, if you’re on digoxin? Please. Don’t even think about switching. I’ve seen two people die from it. One was 72. The other was 34. Both switched generics. Both didn’t make it to the hospital.
Casey Lyn Keller
Did you know the FDA allows generic manufacturers to use different fillers? Like lactose or talc? Some of those fillers can interfere with absorption-especially if you have a sensitive gut. And they don’t have to list them on the bottle. So you think you’re taking the same drug, but your body’s reacting to the filler, not the active ingredient. I’m not saying it’s a conspiracy. I’m saying it’s a loophole. And they’re using it. I’ve been on phenytoin for 18 years. I’ve switched three times. Each time, I had seizures. I’m on the brand now. And I’m not taking a chance again.
Jessica Ainscough
Just want to say thank you for writing this. I’ve been scared to speak up because I thought I was overreacting. I’m on cyclosporine after a kidney transplant. I switched generics once because my insurance forced it. I got a fever, felt nauseous, and my creatinine spiked. I thought it was a virus. Turns out it was the pill. I cried for an hour after the doctor told me. I didn’t know I could be so close to losing my transplant over a $1000 difference. I’m never switching again. And I’m telling everyone I know who’s on NTI drugs to do the same. You’re not being dramatic. You’re being careful. And that’s brave.
Storz Vonderheide
As a pharmacist in rural Ohio, I see this every week. A patient comes in, says their new generic isn’t working. I check the label. It’s the same name as before-but different manufacturer. I call the prescriber. They say ‘dispense as written’-but the patient didn’t know that. We had to go through a 3-day process to get the original back. The system is broken. Pharmacists aren’t the enemy. We’re the last line of defense. But we can’t read minds. We need better labeling. We need mandatory alerts in the system. And we need patients to know their rights. If you’re on an NTI drug, always ask: ‘Is this the same one I got last time?’ If they say yes, ask for the manufacturer name. If they hesitate? Walk out. You’re worth it.
dan koz
Man, this is why I love America. You guys worry about your pills so much. In Nigeria, we just take what we get. If it makes you feel better, it’s good. If it doesn’t, you go to the next pharmacy. No blood tests. No doctors. No stress. I think you need to chill. Life is hard enough without being scared of your own medicine.
Kevin Estrada
Okay but what if the FDA is lying? What if the generics are being secretly modified by Big Pharma to make you dependent on the brand? I’ve been reading forums where people say the same generic from the same manufacturer changes its formula every 6 months. And they don’t tell you. They just change the color. I’m not saying I’m paranoid. I’m saying the system is rigged. I’ve started crushing my pills and mixing them with water so I can see if there’s sediment. If there’s weird stuff? I throw it out. I’m not dying because someone wants to save a buck.
Katey Korzenietz
Just don’t switch. Ever. Done.