Every year, thousands of people die from medication errors. But here's the good news: keeping a simple medication list can prevent most of them. A 2020 study in the Journal of Patient Safety found proper medication reconciliation stops 50-80% of errors during care transitions. That’s over 1.5 million preventable adverse drug events annually. When doctors or pharmacists see your complete medication history, they avoid dangerous interactions. For example, mixing blood thinners with certain painkillers can cause life-threatening bleeding. Your medication list is your personal safety net.
What to Include in Your Medication List
Don’t just write "aspirin" or "blood pressure pill." A useful list has specific details for prescription medications, over-the-counter medications, vitamins, and supplements. For each item, include:
- Full drug name (brand and generic, like "Lisinopril" instead of just "blood pressure medicine")
- Strength (e.g., "10 mg" not "one pill")
- How often you take it (e.g., "once daily at bedtime")
- Why you take it (e.g., "for high blood pressure")
- When you last took it (e.g., "today at 8 AM")
- Prescribing doctor’s name and contact info
The FDA’s "My Medicines" template makes this easy. It has sections for allergies, emergency contacts, and detailed medication entries. Many patients skip OTC drugs or supplements because they think "it’s not real medicine." But that’s dangerous. A 2010 American Heart Association report noted that people often forget to mention herbal teas or fish oil pills during medical visits. These can interact dangerously with prescription drugs.
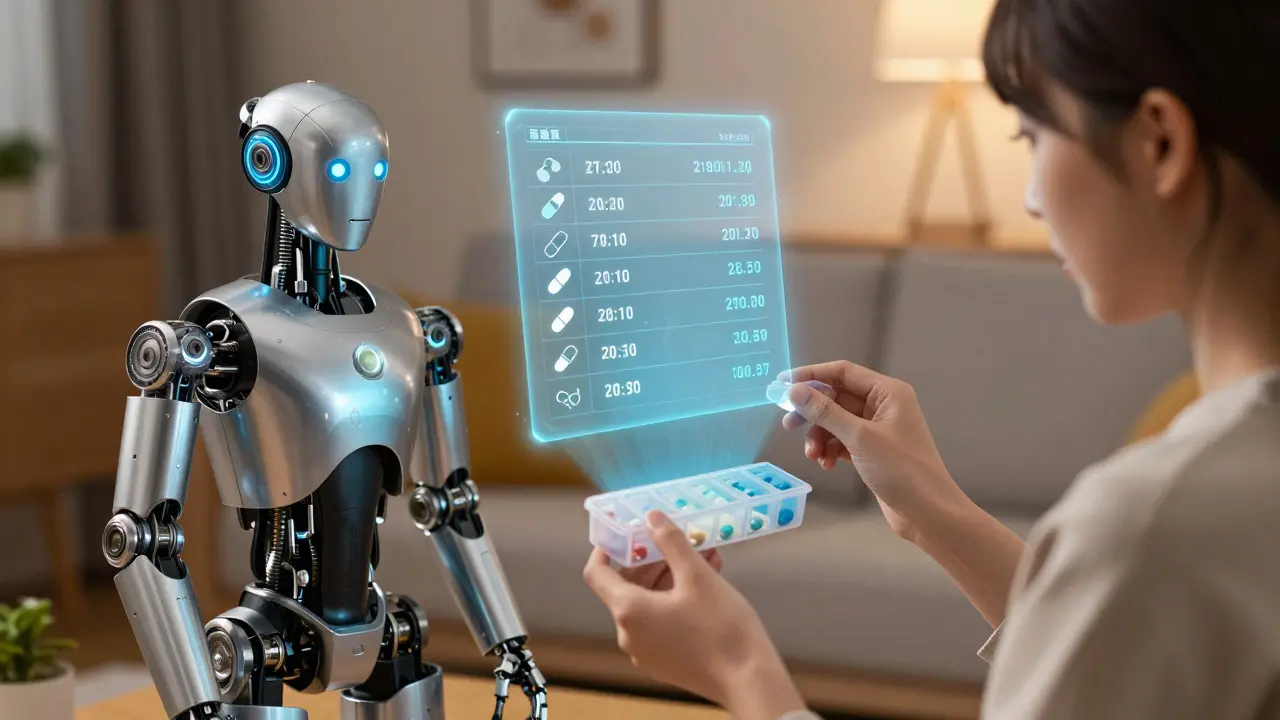
Paper vs. Digital: Which Format Works Best?
You have options for keeping your list. Each has pros and cons. Here’s how they compare:
| Format | Pros | Cons |
|---|---|---|
| Paper | No tech needed; easy to carry | 43% outdated (JAMA 2022 study) |
| Smartphone apps | Automatic refill reminders; 28% fewer missed doses (BMJ Open 2023) | Only 35% of seniors 65+ use them (Pew Research 2023) |
| EHR integration | Real-time updates across hospitals and clinics | 62% of U.S. hospitals use it (AHA 2023) |
Electronic Health Records (EHRs) like Epic Systems’s MyChart let doctors see your list instantly during visits. But if you’re not in a hospital system that uses EHRs, apps or paper work better. For example, Medisafe (used by 6+ million people) sends alerts when it’s time to take pills. MyTherapy has a 4.7/5 rating on Google Play for its simple interface. But if you’re not comfortable with technology, a printed list in your wallet works fine-just update it regularly.

How to Keep Your List Updated
Updating your list is harder than making it. A 2021 University of Michigan study found 68% of patients don’t update their list after hospital discharge. That’s risky-new medications or dose changes can cause errors. Here’s how to stay on top of it:
- Set a weekly reminder on your phone to check your list. For example, every Sunday while organizing your pill box.
- Use the "brown bag method": Before doctor visits, bring all your medicine bottles. Pharmacists can verify what you’re actually taking.
- After any medication change (new prescription, stopping a drug), update your list immediately. Don’t wait.
- Share your list with a family member or caregiver. They can help spot mistakes.
Pharmacists can also help. Medicare Part D covers medication therapy management services for chronic conditions like diabetes or heart disease. A 2023 study in the Journal of General Internal Medicine showed patients who got pharmacist-led education spent just 12.7 minutes per month maintaining their list-half the time of those without training. That’s less time than checking social media!

Common Mistakes and How to Avoid Them
Even with good intentions, people make errors. Here are the top pitfalls:
- Forgetting OTC drugs and supplements: A 2022 Mayo Clinic survey found 53% of patients leave these out. Always include everything-even ginger chews for nausea or melatonin for sleep.
- Not checking for duplicates: Taking two pills with the same active ingredient (like acetaminophen in Tylenol and cold medicine) can cause liver damage. Your list should show exact ingredients.
- Using vague terms: Writing "heart medicine" instead of "Warfarin 5 mg" is useless. Doctors need specifics to avoid mistakes.
- Not sharing it with all providers: If you see a cardiologist and a primary care doctor, give both your updated list. Fragmented care is a top cause of errors.
Dr. Scott Gottlieb, former FDA Commissioner, said in 2022: "Accurate medication lists are the single most important tool for preventing adverse drug events in polypharmacy patients." But he also warned that "over-reliance on patient self-reporting without verification creates false confidence." Always verify your list against pharmacy records or pill bottles.
When to Review Your List
Don’t wait for annual checkups. Review your medication list in these situations:
- Before any surgery or procedure (even dental work)
- After a hospital stay (within 24 hours of discharge)
- When starting a new medication or stopping an old one
- Before seeing a new specialist
- During routine visits with your primary doctor
The Joint Commission requires medication reconciliation at every care transition. This means doctors must compare your list to their records before admitting you or sending you home. A 2022 Kaiser Permanente case study showed this process reduced medication-related readmissions by 22% in just 18 months. For seniors, the National Council on Aging found 67% who kept updated lists reported better communication with doctors. But 41% still forgot to update after changes-so make it a habit.
What if I take dozens of medications?
List every single one-even if it’s 20+ pills. Use the FDA’s "My Medicines" template or a digital app like CareZone. The American Medical Association recommends asking your doctor about "synchronized refills" for chronic conditions. This means getting all prescriptions for 90 days at once, so you only need to update your list four times a year. It saves time and reduces errors.
Can I use a note on my phone?
Yes, but don’t rely on a single text note. Phones can break, get lost, or have forgotten passwords. Use a dedicated app like Medisafe or MyTherapy that syncs across devices. If you use plain notes, keep a printed copy in your wallet too. A 2023 BMJ Open study found app users had 28% fewer missed doses than those using handwritten lists.
How do I handle changes when traveling?
Before trips, review your list with your doctor. Pack medications in their original bottles with labels intact. If you need to refill abroad, show your updated list to a local pharmacist. Carry a physical copy (not just digital) since internet access might be limited. The FDA also recommends noting the generic names of drugs-brand names vary by country. For example, "Lisinopril" is sold as "Zestril" in the U.S. but "Prinivil" elsewhere.
What if my list has errors?
Catch errors early. A 2021 study in JAMA found 56% of patient-reported lists had critical mistakes. If you spot an error (like wrong dose or missing drug), update it immediately and tell all your healthcare providers. Never assume your doctor knows-always share the corrected list. The Institute for Safe Medication Practices says verifying your list with two sources (like pharmacy records and pill bottles) prevents 42% of potential errors. Keep a copy in your car or purse for emergencies.
Do I need to update it after a hospital stay?
Absolutely. Hospitals often change medications during treatment, and 68% of patients forget to update their list after discharge (University of Michigan, 2021). When leaving the hospital, ask for a complete discharge summary with all medication changes. Review it with your primary doctor within 48 hours. The Joint Commission mandates this reconciliation process to prevent readmissions. For example, if you were on blood thinners in the hospital but switched to a new drug, your home list must reflect that change immediately.
9 Comments
jan civil
Last week, pharmacist caught a duplicate cold medicine in my list, preventing liver damage.
Kieran Griffiths
I've been using a medication list for years and it's made a huge difference. It's simple but so effective-just write down every pill you take. I update it every Sunday when I organize my pill box. Including OTC drugs and supplements is critical; I once almost took two different pills with acetaminophen. The brown bag method is great for doctor visits-bring all your bottles. Digital apps like MyTherapy are helpful but I always have a printed copy too. My doctor says it's the single most important thing I can do for my health. It's not rocket science, just a little extra effort. Don't assume your doctor knows your meds-always share the list. Even small things like melatonin can interact with other drugs. I've caught several potential errors this way. It takes less than 5 minutes a week. Trust me, it's worth it. Your health is too important to skip this step.
Joyce cuypers
I update my medication list every Sunday while organizing pills. Including OTCs and supplements has prevented errors before. The brown bag method is great for doctor visits. Oh and I love using the MyMedicines app but sometimes it has typos. It's a lifesaver even with mistakes.
Albert Lua
In India where I'm from people often rely on family for meds. But the FDA template works universally. I've seen how Japan uses digital systems. Adapt to your situation. In my village we have community pharmacists who help manage lists. It's a simple habit that saves lives.
Phoebe Norman
I use a digital app but sometimes forget to update BMJ study says 28% fewer missed doses My doctor says I need to be consistent Medication reconciliation is key. I should check it weekly but life gets busy.
Georgeana Chantie
America is best. Why do we need lists? Other countries should learn from us. 😒 Studies are fake. FDA is always right.
Carol Woulfe
This is a conspiracy by Big Pharma. The FDA template tracks us. I keep my list in a vault. Studies are funded by pharma. It's a scam. The government wants to control us through medication data.
Lisa Scott
This is all nonsense. Studies are manipulated. I don't need a list. My doctor knows my meds. FDA is full of lies. 🤷♂️ The whole system is rigged.
divya shetty
Proper medication lists are crucial for preventing dangerous interactions. In my practice, I've seen cases where patients taking St. John's Wort with warfarin experienced life-threatening bleeding. It's imperative to include all supplements, not just prescription drugs. The FDA's My Medicines template is a simple way to keep track. I recommend updating it weekly, especially after any changes. Many people forget OTC drugs like aspirin or herbal supplements, which can interact with prescriptions. For example, fish oil can increase bleeding risk when combined with blood thinners. Always check with your pharmacist before adding new medications. The Joint Commission requires medication reconciliation at every care transition to prevent errors. A 2022 study in JAMA found 56% of patient-reported lists had critical mistakes. Verifying your list against pharmacy records is essential. I've had patients who didn't update their list after hospital discharge, leading to dangerous omissions. Using a digital app like Medisafe helps, but having a printed copy is also good. Consistency is key-don't wait for annual checkups. This simple habit saves lives every day.