What Are Chemotherapy Hypersensitivity Reactions?
Chemotherapy hypersensitivity reactions are immune system overreactions to cancer drugs. They don’t happen to everyone, but when they do, they can go from mild itching to cardiac arrest in minutes. About 5% of people getting chemotherapy will have some kind of allergic response, and that number climbs the more cycles they receive. Some drugs, like carboplatin and paclitaxel, are far more likely to trigger these reactions than others. The key is knowing what to look for - because early recognition saves lives.
Common Signs and Symptoms by Body System
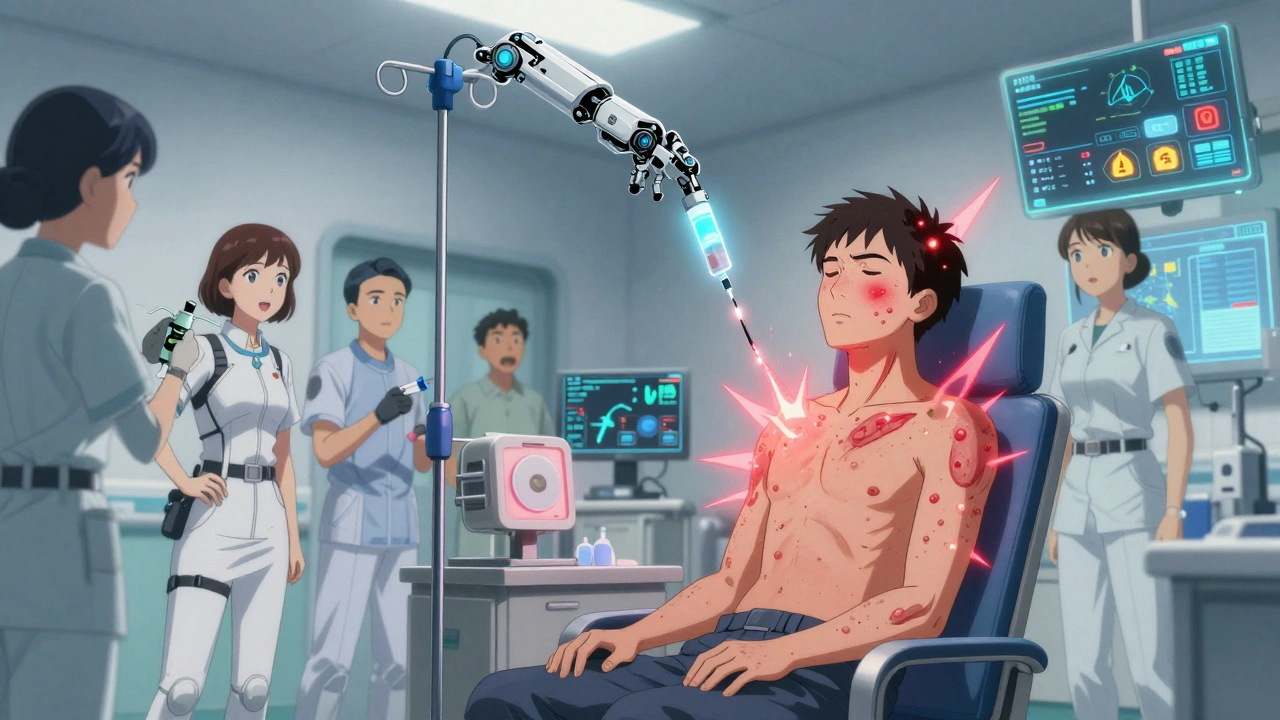
These reactions don’t follow one pattern. They can hit anywhere. Here’s what to watch for, broken down by how they show up in the body.
- Head and neck: Itchy eyes (32% of mild cases), swollen lips or tongue, nasal congestion, tingling in the mouth, or a strange metallic taste.
- Respiratory: Wheezing, coughing, chest tightness, or shortness of breath (45% of moderate reactions). This isn’t just a cold - it’s sudden and worsening.
- Cardiovascular: Dizziness (27%), fainting (18%), rapid heartbeat (HR >100 bpm in 35% of cases), low blood pressure (systolic below 90 mmHg), or even chest pain. These aren’t side effects - they’re warning signs.
- Gastrointestinal: Nausea (35%), vomiting (28%), stomach cramps (42%), or diarrhea (19%). These can be mistaken for chemo nausea, but they come on fast and with other symptoms.
- Skin: Flushing (58%), hives (48%), itching (72%), or rashes. These are often the first visible clues.
- Neurological: Anxiety, a feeling of doom (48% in anaphylaxis), confusion, or even seizures in rare cases.
- Other: Fever (31%), chills (27%), sweating (29%), or vaginal itching (5% of women). These may seem unrelated, but together they form a pattern.
It’s not about one symptom. It’s about the combo. A flushed face and a metallic taste? That’s not just ‘feeling off.’ That’s a red flag.
Which Chemo Drugs Cause the Most Reactions?
Not all chemotherapy drugs are equal when it comes to triggering allergies. Some are far more dangerous than others.
- Platinum drugs: Carboplatin causes reactions in up to 27% of patients after seven cycles. Cisplatin hits 5-20%. Oxaliplatin triggers reactions in nearly 19% of patients, though severe cases are rare (1.6%).
- Taxanes: Paclitaxel and docetaxel are top offenders. Up to 30% of patients react, especially if they haven’t had premedication.
- Liposomal doxorubicin, L-asparaginase, procarbazine, etoposide, bleomycin, cytarabine: These all carry notable risk, with L-asparaginase and cytarabine among the highest.
- Monoclonal antibodies: Cetuximab, rituximab, trastuzumab - these biologics can cause reactions even on the first dose.
The risk isn’t random. It builds up. With carboplatin, the chance of a reaction jumps from less than 1% in the first five cycles to 44% if you’re getting it for the third time. That’s not a fluke - it’s a pattern.
When Do Reactions Happen?
Timing matters. Most reactions occur during the infusion or within the first hour after. But they can also show up 1-2 days later. That’s why patients need to be told: if something feels wrong after you leave the clinic, call back.
Infusion reactions usually start after the second or third cycle. But carboplatin is different. It doesn’t strike early - it sneaks up after multiple doses. That’s why people think they’re fine until suddenly, they’re not.
Speed of infusion plays a role too. Giving the drug too fast means it hits the bloodstream all at once. That’s when mast cells explode with histamine - and symptoms follow in seconds.
How Are These Reactions Diagnosed?
Doctors don’t guess. They look for clear signs: sudden onset, involvement of two or more body systems, and no other explanation.
Lab tests help confirm it:
- High serum tryptase (>11.4 ng/mL) - a marker of mast cell activation.
- Elevated eosinophils (>500 cells/μL) - suggests allergic inflammation.
- Basophil activation tests - measure CD63 or CD203c markers on immune cells.
- Allergen-specific IgE testing - for certain drugs, like monoclonal antibodies.
But diagnosis isn’t just about labs. It’s about context. Is the patient on a known high-risk drug? Did symptoms start during infusion? Are there multiple systems involved? If yes, treat it as anaphylaxis until proven otherwise.
Don’t confuse it with septic shock or asthma. Both can mimic chemo reactions. But sepsis usually has fever and low white blood cells. Asthma doesn’t cause flushing or low blood pressure. The pattern tells the story.
Emergency Management: What to Do When a Reaction Happens
There’s no time for hesitation. Here’s what happens step by step.
Mild Reaction (Grade 1)
Flushing, mild rash, localized itching. No breathing or blood pressure issues.
- Stop the infusion immediately.
- Give diphenhydramine (25-50 mg IV).
- Give dexamethasone (10-20 mg IV).
- Monitor vitals every 5 minutes.
- If symptoms resolve in 15-30 minutes, restart infusion slowly - at half the original rate.
Moderate Reaction (Grade 2)
Widespread hives, facial swelling, mild wheezing, or nausea.
- Stop the infusion.
- Give diphenhydramine and dexamethasone.
- Administer oxygen (4-6 L/min via nasal cannula).
- Keep patient lying flat with legs elevated if dizzy or low on blood pressure.
- Do not restart the same drug on the same day. Wait 24 hours and restart at 25% speed only if symptoms fully resolved.
Severe Reaction (Grade 3-4) - Anaphylaxis
Hypotension, bronchospasm, angioedema, loss of consciousness, cardiac arrest.
- Stop the infusion. Call for emergency help immediately.
- Give epinephrine (0.3-0.5 mg of 1:1,000 solution) into the outer thigh muscle. Repeat every 5-15 minutes if needed.
- Start IV fluids - 1-2 liters of normal saline.
- Give oxygen. Prepare for intubation if airway is swelling.
- Give methylprednisolone (125 mg IV) and diphenhydramine.
- Monitor continuously for at least 24 hours - reactions can rebound.
Angioedema of the tongue or throat? That’s an airway emergency. Don’t wait. Give epinephrine and get help. Delaying means death.
Prevention: How to Avoid Reactions Before They Start
Prevention isn’t optional - it’s standard care for high-risk drugs.
For taxanes (paclitaxel, docetaxel), premedication is mandatory:
- Dexamethasone: 20 mg IV, 12 hours and 6 hours before infusion.
- Diphenhydramine: 50 mg IV, 30 minutes before.
- Famotidine: 20 mg IV, 30 minutes before.
Slowing the infusion rate helps too. First-time paclitaxel? Start at 1 mg/min. If no reaction, increase slowly.
For carboplatin, avoid rushing. Even if the patient had no reaction before, assume risk is rising with each cycle. Consider switching to cisplatin or oxaliplatin after multiple reactions.
And always - always - ask patients: Have you ever had an allergic reaction to chemo before? If yes, document it. If they say ‘no,’ ask again. Sometimes they forget. Sometimes they think it was just ‘bad nausea.’
What Happens After a Reaction?
If someone has a severe reaction, they usually can’t get that drug again. But if the chemo is critical - and there’s no alternative - desensitization is an option.
Desensitization means giving the drug in tiny, increasing doses over 4 to 12 hours. It’s done under constant monitoring, with emergency drugs ready. It works for many patients - but only if the reaction wasn’t life-threatening. If they had cardiac arrest or airway closure, the risk is too high.
After any reaction, the patient’s chart must be flagged. All future providers must know: ‘Do not re-administer [drug name].’
Why This Matters - The Human Side
Patients don’t always know what they’re feeling. They might say, ‘I just feel weird,’ or ‘My face is hot.’ Nurses and doctors need to listen - not dismiss it as anxiety or side effects.
One woman in Leeds came in for her sixth carboplatin cycle. She said, ‘My mouth feels funny.’ The nurse paused the drip. Five minutes later, her lips swelled. She was given epinephrine. She’s alive today because someone listened.
Another patient thought her wheezing was just asthma. She didn’t tell anyone. By the time she collapsed, it was too late.
These reactions are rare - but deadly. And they’re preventable. Not with fancy tech. With attention. With training. With courage to stop the drip when something feels off.
Final Takeaway
Chemotherapy hypersensitivity isn’t rare. It’s predictable. It’s documented. It’s manageable - if you know the signs, know the drugs, and know the protocol.
Don’t wait for a textbook case. If a patient says something feels wrong - believe them. Check their vitals. Stop the infusion. Give epinephrine if needed. Don’t overthink it. Underreacting kills. Overreacting saves lives.
Every oncology unit should have an anaphylaxis kit within arm’s reach. Every nurse should know where it is. Every patient should know to speak up - even if they’re scared.
Can chemotherapy hypersensitivity reactions happen on the first treatment?
Yes. While some reactions build up over multiple cycles - like with carboplatin - others, especially with monoclonal antibodies like cetuximab or rituximab, can occur on the very first infusion. That’s why all patients are monitored closely during their first treatment, even if they’ve never had an allergic reaction before.
Is it safe to use the same chemo drug again after a mild reaction?
Sometimes. If the reaction was mild - like flushing or a small rash - and fully resolved after stopping the infusion and giving antihistamines, doctors may restart the drug at a slower rate with premedication. But if symptoms returned or worsened, the drug is usually avoided permanently. Always consult an oncology pharmacist or allergist before re-challenging.
What’s the difference between an infusion reaction and a true allergic reaction?
Infusion reactions are often caused by the body’s direct response to the drug - like cytokine release - and don’t involve IgE antibodies. True allergic reactions are immune-mediated, meaning the body has made antibodies against the drug. Both can look the same: flushing, fever, breathing trouble. But only true allergies show up on IgE or tryptase tests. In practice, you treat both the same way - because the symptoms are deadly either way.
Can antihistamines alone stop a severe chemo reaction?
No. Antihistamines help with itching and hives, but they do nothing for low blood pressure, airway swelling, or cardiac arrest. Epinephrine is the only drug that reverses anaphylaxis. Delaying epinephrine to give more antihistamines can be fatal. If there’s any sign of shock or breathing trouble, give epinephrine immediately - don’t wait.
Are there any long-term risks after surviving a chemo hypersensitivity reaction?
Most patients recover fully if treated quickly. But those who had severe reactions may need to avoid the drug forever, which can limit treatment options. Some develop new sensitivities to other drugs or contrast dyes. Long-term, the biggest risk is not the reaction itself - it’s being denied effective cancer treatment because the right alternative isn’t available.
Should patients carry an epinephrine auto-injector after a chemo reaction?
Not routinely. Chemo reactions happen in controlled settings where emergency care is available. But if a patient has a history of severe anaphylaxis and is being treated with a drug that can’t be easily switched - or if they’re at high risk for future reactions - some specialists may prescribe an auto-injector for use outside the clinic. This is rare and decided case-by-case with an allergy specialist.
11 Comments
Nicholas Heer
soooooo... are we just gonna ignore the fact that Big Pharma *wants* us to have these reactions? I mean, think about it - if you get a reaction, you need MORE drugs to fix it. More steroids. More epinephrine. More $$$ for the hospital. And guess who owns the patents on all those meds? Same corporations that make the chemo. Coincidence? I think not. They profit off your suffering. Wake up.
Sangram Lavte
This is one of the most thorough breakdowns I've seen on chemo reactions. The breakdown by body system is especially helpful. I’ve seen patients miss early signs because they thought it was just 'chemo fatigue.' This should be mandatory reading for all oncology nurses.
Oliver Damon
The distinction between infusion reactions and true IgE-mediated hypersensitivity is clinically vital but often blurred in practice. The pathophysiology differs - one’s a cytokine storm, the other’s mast cell degranulation - yet both demand identical emergency responses. That’s the irony: biology demands precision, but survival demands simplicity. We treat them the same because the cost of overthinking is death. The protocol isn’t perfect - it’s pragmatic.
Kurt Russell
LISTEN UP. If you’re a nurse, a doctor, or a caregiver - STOP WAITING. If a patient says their mouth feels funny, their face is hot, or they have a metallic taste - YOU STOP THE INFUSION. NO EXCUSES. I’ve seen people die because someone said 'it’s probably just anxiety.' It’s not. It’s anaphylaxis. And epinephrine doesn’t wait. Give it. Now. Your hesitation is their coffin.
Stacy here
They say 'trust your gut' - but in oncology, your gut is the only thing that hasn't been poisoned yet. I had a friend who got carboplatin for 5 cycles with zero issues. Then on cycle 6, she said 'I feel like I'm melting.' They laughed. She had angioedema. They intubated her at 3am. She survived. But what if they hadn't listened? The system doesn't train people to believe patients - it trains them to believe protocols. And protocols don't scream. People do.
Kyle Flores
I work in a small clinic and we don't always have the luxury of a full code team. That’s why I keep an epinephrine auto-injector in the chemo bay - just in case. I know it’s not standard, but I’d rather be called overcautious than guilty. If you’re reading this and you’re not prepared - fix it. One life is worth more than policy.
Ryan Sullivan
Let’s be real - most of this is common sense. If your patient turns into a red balloon and starts wheezing, you don’t need a 20-page protocol to know something’s wrong. The real problem? Overworked staff, undertrained aides, and hospitals that cut corners to save $200 on an epinephrine kit. This isn’t science. It’s negligence dressed up as guidelines.
Wesley Phillips
So basically if your face feels weird after chemo, you’re gonna die unless you scream for epinephrine? Cool. I’m just glad I’m not the one getting this stuff. Also, why is everyone so obsessed with carboplatin? Like, I get it, it’s a common drug - but are we really supposed to panic every time someone says 'my tongue tingles'? Chill. It’s probably just the salt in the IV fluid.
Olivia Hand
I’m curious - how many of these reactions are misdiagnosed as anxiety, especially in women? The data shows flushing and metallic taste are common, yet women are often told they're 'overreacting' or 'stressed.' Is there any study looking at gender bias in chemo reaction recognition?
Desmond Khoo
This is why I love real medical content 🙌 I’ve been through chemo twice and no one ever told me about the metallic taste or the 'feeling of doom' - I thought I was losing my mind. This post saved me from panic. If you’re on chemo - read this. Save yourself. You got this 💪
Louis Llaine
Wow. 12 pages of 'stop the drip' and 'give epinephrine.' Groundbreaking. Next up: 'Water is wet, and fire burns.' Someone get this man a Nobel Prize for discovering that allergic reactions are bad.