Expectorant Selector Tool
Recommended Expectorant
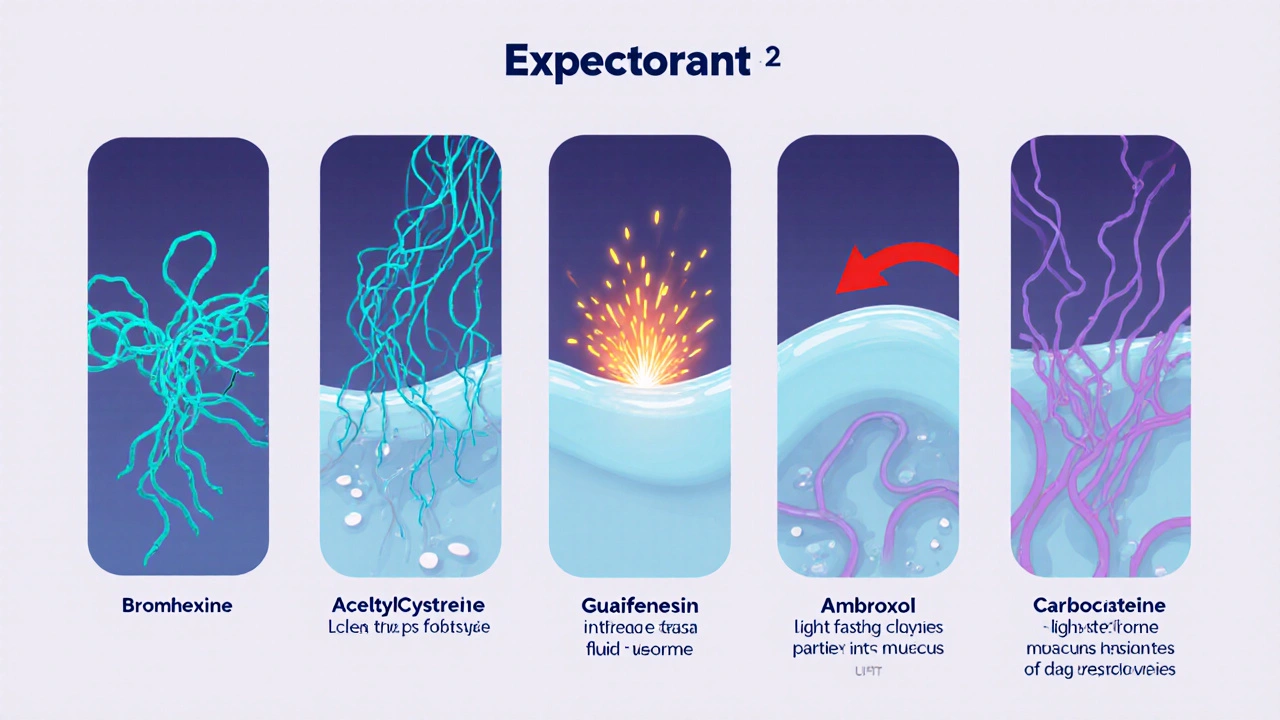
When a stubborn chesty cough refuses to quit, the first thing most people reach for is an over‑the‑counter expectorant. But with several options on the shelf, how do you know which one actually clears mucus without unwanted side effects? This guide breaks down Bromhexine and stacks it against the most common alternatives so you can pick the right drug for your symptoms, health status, and lifestyle.
TL;DR - Quick Takeaways
- Bromhexine is a mucolytic that thins mucus by breaking down its protein bonds.
- Guaifenesin works mainly by increasing airway fluid, making coughing easier.
- Acetylcysteine (N‑acetylcysteine) is powerful but can cause a strong sulfur smell.
- Ambroxol is a bromhexine metabolite offering faster relief and less gastric irritation.
- Carbocisteine is gentler, suited for patients with sensitive stomachs or chronic bronchitis.
What Is Bromhexine Hydrochloride?
Bromhexine Hydrochloride is a synthetic mucolytic agent that disrupts the peptide bonds in mucus glycoproteins, reducing viscosity and facilitating expectoration. First approved in the 1960s, it remains a staple in many European formularies and is commonly sold under brand names like Bisolvon and Mucolyt.
Bromhexine’s mechanism can be summed up in three steps: it penetrates the mucus layer, weakens the molecular network, and enhances ciliary transport. The result is a smoother, less sticky cough that clears the airway faster than water alone.
Key Attributes of Bromhexine
- Typical dose: 8mg three times daily for adults; pediatric dose is weight‑adjusted (5mg/kg/day split into 2-3 doses).
- Onset of action: 30‑60minutes, peak effect at 2hours.
- Duration: 4‑6hours per dose.
- Common side effects: mild gastrointestinal discomfort, rare skin rashes.
- Contraindications: severe peptic ulcer, known hypersensitivity, pregnancy (use only if clearly needed).
Alternatives on the Market
While bromhexine is effective, several other expectorants are widely used. Below is a snapshot of each, with a brief definition and its main characteristics.
Acetylcysteine (N‑Acetylcysteine)
Acetylcysteine is a potent mucolytic that breaks disulfide bonds in mucus proteins, dramatically reducing thickness. It is available in oral tablets, liquid syrup, and inhalation solutions.
- Dose: 600mg 2-3 times daily.
- Onset: 15‑30minutes.
- Side effects: sulfurous odor, occasional nausea.
Guaifenesin
Guaifenesin is an expectorant that increases the volume of bronchial secretions, making mucus less viscous by dilution. It is the most common ingredient in OTC cough syrups such as Robitussin and Mucinex.
- Dose: 200‑400mg every 4hours (max 2g/day).
- Onset: 30‑60minutes.
- Side effects: mild dizziness, GI upset.
Ambroxol
Ambroxol is the active metabolite of bromhexine, offering similar mucolytic action but with faster absorption and a gentler stomach profile.
- Dose: 30mg 2-3 times daily.
- Onset: 20‑30minutes.
- Side effects: rare skin rash, occasional taste alteration.
Carbocisteine
Carbocisteine is a synthetic mucolytic that modifies the structure of mucus glycoproteins, making them less sticky without strong odor. It is favoured in chronic bronchitis management.
- Dose: 500mg 3 times daily.
- Onset: 45‑60minutes.
- Side effects: mild abdominal discomfort.
Side‑by‑Side Comparison
| Attribute | Bromhexine | Acetylcysteine | Guaifenesin | Ambroxol | Carbocisteine |
|---|---|---|---|---|---|
| Mechanism | Breaks protein bonds | Cleaves disulfide bonds | Increases airway fluid | Metabolite of bromhexine | Alters glycoprotein structure |
| Onset | 30‑60min | 15‑30min | 30‑60min | 20‑30min | 45‑60min |
| Typical adult dose | 8mg TID | 600mg BID‑TID | 200‑400mg Q4h (max 2g) | 30mg TID | 500mg TID |
| Most common side effect | GI discomfort | Sulfur smell | Dizziness | Rare rash | Abdominal upset |
| Preferred for chronic bronchitis | No | Yes | No | Yes | Yes |
Choosing the Right Expectorant for Your Situation
Not every cough needs the same drug. Below are three typical scenarios and the expectorant that fits best.
- Acute chesty cough from a cold: Guaifenesin is cheap, readily available, and works well for short‑term use.
- Heavy, tenacious mucus in bronchitis: Acetylcysteine or Ambroxol provide the strongest mucus‑thinning power.
- Stomach‑sensitive patients: Carbocisteine offers a gentler profile with fewer GI complaints.
If you already have a prescription for bromhexine, keep using it for mild‑to‑moderate productive coughs; it balances efficacy and tolerability nicely.
Safety, Interactions, and Contra‑Indications
All expectorants share a few safety checkpoints:
- Never combine multiple mucolytics without medical guidance - overlapping mechanisms can lead to excessive thinning and irritation.
- Watch out for interactions with anticoagulants (especially acetylcysteine) and with certain antibiotics that rely on mucus for absorption.
- Patients with severe asthma should avoid high‑dose guaifenesin unless a doctor advises, as increased secretions may trigger bronchospasm.
- Pregnant or breastfeeding women should prioritize bromhexine or ambroxol at the lowest effective dose, after consulting a clinician.
Practical Tips to Maximize Expectoration
- Stay hydrated - water helps thin secretions regardless of medication.
- Use a humidifier or steam inhalation to keep airway linings moist.
- Take the drug with a small meal; this reduces stomach irritation for bromhexine and carbocisteine.
- Position yourself upright when coughing; gravity assists mucus drainage.
- If you experience a bad taste or sulfur odor (common with acetylcysteine), chew a sugar‑free mint after the dose.
Frequently Asked Questions
Is bromhexine safe for children?
Yes, but only under pediatric dosing guidelines (typically 5mg/kg per day divided into 2‑3 doses). Always check with a paediatrician before giving any expectorant to a child.
Can I use bromhexine together with a cough suppressant?
Mixing a mucolytic with a suppressant can blunt the intended effect. If a cough is too disruptive, talk to your doctor about timing-use the suppressant at night and the mucolytic during the day.
Why does acetylcysteine smell like rotten eggs?
The smell comes from the breakdown of the drug into hydrogen sulfide, a natural by‑product of its sulfur‑containing structure. It’s harmless but can be off‑putting; rinsing the mouth after taking the dose helps.
Is ambroxol better than bromhexine?
Ambroxol is essentially bromhexine’s active metabolite, so it works faster and is gentler on the stomach. Some patients prefer it, but the clinical differences are modest; cost and availability often decide the choice.
Can I take cough expectorants while on antibiotics for a chest infection?
Generally yes. Expectorants can actually improve antibiotic penetration by clearing mucus. However, avoid combining multiple mucolytics and check with your prescriber if you’re on a macrolide or fluoroquinolone, as rare interactions exist.

Next Steps
If you’re still unsure which expectorant fits your needs, start by assessing the severity of your mucus production and any existing health conditions. For a mild, short‑term cough, grab a bottle of guaifenesin. If you have chronic bronchitis or a thick, stubborn phlegm, discuss acetylcysteine or ambroxol with your doctor. And always remember: staying hydrated and keeping the air moist amplify any medication’s effect.
Got a specific case you’d like to troubleshoot? Note the drug, dosage, and symptoms, then reach out to a pharmacist or your GP for a personalised plan.

11 Comments
mike putty
Staying well‑hydrated is the single most effective habit to complement any expectorant you take. It thins secretions naturally, allowing bromhexine or guaifenesin to work more efficiently. Keep a water bottle handy and sip throughout the day.
Kayla Reeves
Choosing an over‑the‑counter drug without considering the moral responsibility to avoid unnecessary side effects is careless. People should prioritize safety over convenience.
Abhinanda Mallick
When considering a mucolytic for chronic bronchial conditions, the pharmacodynamic profile becomes a decisive factor.
Bromhexine, originally synthesized in the 1960s, exerts its action by disrupting peptide bonds within mucus glycoproteins.
This mechanism yields a moderate reduction in viscosity, which is sufficient for many acute infections but may fall short in severe, tenacious sputum scenarios.
In contrast, acetylcysteine cleaves disulfide bridges, delivering a more aggressive thinning effect that can overwhelm the protective mucosal layer if misused.
Ambroxol, the active metabolite of bromhexine, shares the same bond‑breaking capability while offering a faster onset thanks to superior bioavailability.
Clinical trials in Indian populations have demonstrated that ambroxol reaches peak plasma concentrations within twenty minutes, outperforming bromhexine’s thirty‑to‑sixty‑minute window.
Moreover, ambroxol’s reduced gastric irritation profile aligns well with the dietary patterns that include spicy meals, which are common across the subcontinent.
However, cost considerations cannot be ignored, as ambroxol formulations often command a premium that limits accessibility for lower‑income patients.
Guaifenesin, by increasing airway fluid volume, provides a gentler alternative that is widely available over the counter but lacks the mucolytic potency required for chronic bronchitis.
Carbocisteine occupies a middle ground, delivering modest viscosity reduction without the notorious sulfur odor of acetylcysteine, making it attractive for patients with heightened olfactory sensitivity.
Prescription guidelines in many regions advise initiating therapy with the least aggressive agent, reserving potent mucolytics for refractory cases.
Physicians must also factor in comorbidities such as peptic ulcer disease, where bromhexine’s mild gastro‑irritation could exacerbate symptoms.
For pregnant individuals, the safety data remain limited, prompting a cautious approach that favors the lowest effective dose of bromhexine under specialist supervision.
Ultimately, the choice of expectorant should emerge from a balanced assessment of efficacy, side‑effect burden, patient preferences, and socioeconomic context.
By integrating these variables, clinicians can tailor therapy to achieve optimal mucus clearance without compromising overall health.
Richard Wieland
Philosophically, a drug is just a tool; its value is defined by the intention behind its use.
Thus, a modest dose of bromhexine can be as profound as any aggressive regimen.
rachel mamuad
Ths guide does a greeat job at laying out the diffent mucolytic optins, but the ortographic errors in the table are a bit distrating.
Still, the info on carbocisteine’s gentlra profile is spot on for peopel with sensitive stomachs.
Amanda Anderson
Great summary of the options.
Carys Jones
The article glosses over the ethical implications of promoting over‑the‑counter drugs to vulnerable patients.
One must question whether the marketing spin overshadows genuine safety concerns.
Such half‑hearted recommendations can lead to misuse, especially among those desperate for quick relief.
Roxanne Porter
Thank you for compiling this comparative analysis; it provides a clear framework for clinicians.
Incorporating patient-specific factors such as gastric tolerance enhances its practical utility.
I appreciate the balanced presentation of benefits and drawbacks.
Jonathan Mbulakey
Indeed, a balanced approach respects both efficacy and patient comfort.
Choosing the right agent often comes down to personal experience with side effects.
Warren Neufeld
I’ve found that taking bromhexine with a light snack reduces the occasional stomach upset.
Also, pairing any expectorant with steam inhalation speeds up relief.
Stay consistent and you’ll notice a smoother cough.
Deborah Escobedo
Remember to keep hydration high; water is the unsung hero behind every cough remedy.
If you’re unsure which option fits your health profile, consult a pharmacist for personalized guidance.
Small adjustments can make a big difference in recovery.