Many older adults reach for over-the-counter antihistamines like Benadryl to help with allergies, colds, or sleep. It’s cheap, easy to find, and seems harmless. But what if taking it every night for years could quietly raise your risk of memory problems? That’s the growing concern behind antihistamines and dementia risk - especially when it comes to first-generation drugs like diphenhydramine and doxylamine.
How Antihistamines Affect the Brain
Not all antihistamines are the same. First-generation ones - such as diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine - cross the blood-brain barrier. Once inside, they block acetylcholine, a key brain chemical needed for memory, attention, and learning. This is called anticholinergic activity. It’s why these drugs make you drowsy. But over time, constantly reducing acetylcholine may interfere with how brain cells communicate, potentially contributing to cognitive decline. Second-generation antihistamines - like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) - were designed to avoid this. They don’t cross into the brain easily because of special transporters that push them out. As a result, their anticholinergic effect is 100 to 1,000 times weaker. For someone needing daily allergy relief, switching to one of these is a simple, low-risk change.What the Research Actually Shows
A 2015 study in JAMA Internal Medicine that tracked over 3,400 adults aged 65+ for 10 years sparked widespread concern. It found a link between long-term use of anticholinergic drugs and higher dementia risk. But here’s the twist: when researchers looked at antihistamines alone, the risk wasn’t clear. Other drugs - like certain antidepressants, bladder medications, and Parkinson’s drugs - showed stronger associations. In fact, a 2019 follow-up study found no significant dementia risk tied specifically to antihistamine use (hazard ratio of 1.00). A 2022 study of nearly 9,000 older adults showed higher dementia rates among those using first-gen antihistamines (3.83%) compared to second-gen users (1.0%). But even that difference wasn’t statistically significant after adjusting for other factors. That means the data doesn’t prove one caused the other. It just shows they sometimes happen together. Why the confusion? Many studies group all anticholinergics together. When you mix drugs with strong brain effects (like oxybutynin for overactive bladder) with mild ones (like Claritin), the signal gets blurred. Also, people who take these meds often have other health issues - chronic allergies, insomnia, depression - that themselves may raise dementia risk. So is it the drug, or the underlying condition?Expert Guidelines Are Clearer Than the Science
Despite mixed evidence, medical organizations are acting cautiously. The American Geriatrics Society’s 2023 Beers Criteria, a trusted guide for prescribing in older adults, says: avoid first-generation antihistamines in people 65 and older. They give diphenhydramine the highest warning level (Level A) - meaning the risk is well-documented and the recommendation is strong. The Anticholinergic Cognitive Burden Scale (ACB) rates diphenhydramine as a 3 - the worst possible score. Fexofenadine and loratadine? Score 0. That’s why doctors are increasingly switching patients off Benadryl for sleep or allergies. The American Academy of Neurology recommends reviewing all medications every six months and choosing alternatives whenever possible. Meanwhile, the European Medicines Agency updated patient leaflets in 2022 to include a note about “potential long-term cognitive effects with prolonged use.” The FDA, however, still only requires OTC labels to say “may cause drowsiness.” There’s a gap between what experts know and what consumers see on the bottle.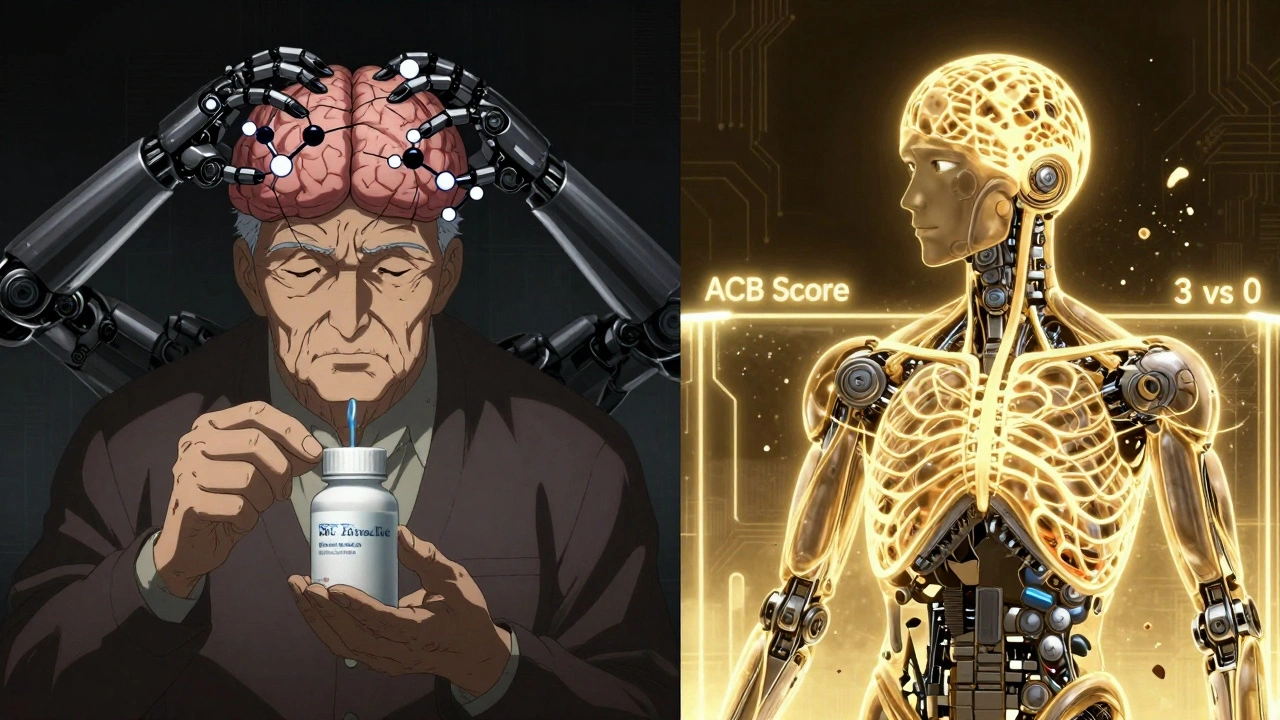
Who’s Most at Risk?
Not everyone who takes Benadryl will develop dementia. But some people are more vulnerable:- Those over 70
- People taking multiple anticholinergic drugs (e.g., Benadryl + a bladder med + an antidepressant)
- Individuals with mild cognitive impairment or early memory complaints
- Those using these drugs daily for more than three years
What to Do Instead
If you or a loved one is using diphenhydramine for sleep or allergies, here’s what to consider:For allergies: Switch to loratadine, cetirizine, or fexofenadine. They work just as well without the brain fog. No prescription needed.
For sleep: Benadryl isn’t meant for long-term insomnia. It disrupts sleep architecture, leading to poor-quality rest. Better options:
- Cognitive Behavioral Therapy for Insomnia (CBT-I): Proven effective in 70-80% of older adults. It teaches better sleep habits without drugs.
- Low-dose doxepin (Silenor): A prescription sleep aid with minimal anticholinergic activity (ACB score of 1).
- Non-drug strategies: Reduce screen time before bed, keep a consistent sleep schedule, avoid caffeine after noon, and get sunlight in the morning.
CBT-I works better than pills for long-term results - but access is limited. Average wait time for a therapist is over eight weeks, and Medicare only covers $85-$120 per session. Still, it’s a safer investment than years of daily anticholinergics.
The Bigger Picture: Why This Matters
The global market for first-gen antihistamines dropped 24% between 2015 and 2022. Sales of second-gen versions rose 18% in the same period. That’s not coincidence. As awareness grows, people are switching. Pharmaceutical companies are responding with newer, safer alternatives. The NIH is funding a major 10-year study called ABCO, tracking 5,000 older adults to get clearer answers. Early data from the UK Biobank suggests that when researchers account for underlying sleep disorders, the link between antihistamines and dementia disappears. That’s a big clue - maybe the problem isn’t the drug, but the reason people take it. Still, the American Geriatrics Society doesn’t wait for perfect data. They act on what’s known now. And what’s known is that first-gen antihistamines carry a real, avoidable risk - especially in older adults.Final Takeaway
If you’re over 65 and taking Benadryl, Unisom, or any OTC sleep aid with diphenhydramine or doxylamine as the active ingredient - pause. Ask yourself: Why am I taking this? How long have I been taking it? Is there a safer option? Switching to a second-generation antihistamine for allergies is easy. Finding a better solution for sleep takes more effort - but it’s worth it. Your brain will thank you.Can antihistamines cause dementia?
There’s no definitive proof that antihistamines directly cause dementia. But long-term use of first-generation types like diphenhydramine is linked to higher risk in some studies, likely because they block acetylcholine - a brain chemical vital for memory. Experts recommend avoiding them in older adults not because they definitely cause dementia, but because safer alternatives exist and the potential harm isn’t worth the risk.
Is Benadryl safe for seniors?
No, Benadryl (diphenhydramine) is not considered safe for long-term use in seniors. The American Geriatrics Society advises avoiding it entirely in adults 65+ due to its high anticholinergic burden. It can cause confusion, dizziness, urinary retention, and may contribute to cognitive decline over time. Safer options are available for both allergies and sleep.
What are the safest antihistamines for older adults?
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are the safest choices. They treat allergies effectively without crossing into the brain or blocking acetylcholine. They don’t cause drowsiness in most people and carry no anticholinergic risk according to the ACB scale.
Can I stop taking Benadryl cold turkey?
If you’ve been using Benadryl daily for sleep or allergies, don’t stop suddenly without talking to your doctor. While it’s not addictive, your body may have adapted to it. Stopping abruptly could cause rebound symptoms like worse allergies or temporary insomnia. Work with your provider to switch to a safer alternative gradually.
Does Claritin or Zyrtec increase dementia risk?
No. Studies show no increased dementia risk with loratadine (Claritin) or cetirizine (Zyrtec). These second-generation antihistamines have minimal to no anticholinergic activity because they don’t enter the brain in significant amounts. They are recommended as safer alternatives for older adults who need daily allergy relief.
How long does it take for anticholinergic effects to impact memory?
There’s no exact timeline, but research suggests risk increases with cumulative exposure over years - especially beyond three years of daily use. The effect is likely gradual, with subtle memory changes building over time. That’s why experts stress regular medication reviews: catching long-term use early gives you time to switch safely.

9 Comments
AARON HERNANDEZ ZAVALA
I used to take Benadryl every night for years just to fall asleep. Never thought twice about it until my grandma got diagnosed with early dementia and I started reading up on meds. Now I feel kind of guilty. Switched to Zyrtec for allergies and melatonin for sleep. No brain fog anymore. Feels like my mind cleared up after 2 weeks.
Victor T. Johnson
Stop being dramatic. You think your brain is fragile because you took a little diphenhydramine? 😂 My grandpa took Benadryl for 40 years and still beats me at chess. The real cause of dementia? Sugar. Processed food. Sitting on your ass watching Netflix. Not a $5 OTC pill. Wake up.
Nicholas Swiontek
Hey everyone - I work in a senior care center and this is 100% real. We’ve had multiple cases where switching from Benadryl to Claritin made patients noticeably more alert, less confused, even more engaged at meals. It’s not magic, it’s just removing a brain depressant. Small change, huge difference. 🙌
Robert Asel
It is imperative to recognize that the causal inference drawn from observational epidemiological studies is inherently confounded by indication bias. The conflation of correlation with causation in this context is a textbook example of ecological fallacy. The anticholinergic burden scale, while useful for pharmacological classification, does not constitute clinical proof of neurodegenerative causality. One must consider the multivariate nature of cognitive decline.
Shannon Wright
Let me tell you something - I’m a nurse and I’ve seen this over and over again. Older adults are given Benadryl for sleep because it’s cheap, easy, and the doctor doesn’t want to spend time explaining alternatives. But then they come back six months later saying they’re foggy, forgetful, and can’t remember their grandkids’ names. It’s not the dementia that’s the problem - it’s that we’ve normalized putting people to sleep with brain-slowing drugs instead of helping them sleep better. CBT-I isn’t just a therapy - it’s a gift. And yes, wait times are long. But if you start now, you might beat the queue. Your future self will thank you.
vanessa parapar
Oh please. If you’re still taking Benadryl after 65, you’re basically asking for dementia. I told my uncle three times to stop and he didn’t listen. Now he can’t remember his own birthday. Classic. Zyrtec is free at CVS with a coupon. Do the thing.
Ben Wood
I’ve read the JAMA study. The 2019 follow-up. The ACB scale. The Beers Criteria. The UK Biobank data. The NIH ABCO trial. And yet - you’re all acting like this is new news? This has been known since the 90s. The FDA doesn’t regulate OTC like it should. Pharmaceutical companies don’t want you to know. Your doctor? Probably still prescribing it. You’re not just ignorant - you’re complicit. And yes, I’m talking to you, Benadryl-nightly-user. You’re the problem.
Sakthi s
Switch to cetirizine. Easy. Safe. Done.
Rachel Nimmons
They’re hiding the truth. The same people who told you Benadryl was safe are the ones pushing vaccines, GMOs, and fluoride. Why do you think they don’t want you to know? Because if you stop taking it, they lose control. I’ve been tracking this since 2012. The cognitive decline? It’s not the drug - it’s the microchips in the pills. They’re watching. They’re testing. Don’t be the next one to wake up confused.